The Journal of Clinical and Preventive Cardiology has moved to a new website. You are currently visiting the old
website of the journal. To access the latest content, please visit www.jcpconline.org.
Original Article
Epidemiological and Clinical Profile of Pulmonary Hypertension: Data from an Indian Registry
Volume 1, Apr 2012
Rahul Mehrotra, MD, DNB, Manish Bansal, MD, DNB, Ravi R Kasliwal, MD, DM; Naresh Trehan, MD, Gurgaon, India
Volume 1, April 2012
Pulmonary hypertension (PH) is one of the most devastating disorders of the cardiovascular system associated with poor survival and considerable morbidity. The disease has largely remained obscure on account of several factors. Although it was known almost 100 years ago (1), most of the knowledge related to the disease has evolved during the last 25 years or so. The diagnostic criteria, classification, and even nomenclature have undergone several changes in this period (the term primary PH being replaced by idiopathic PH). That there is no single causative factor and PH may represent the final common pathway for myriad diseases (ranging from collagen vascular diseases to infection with human immune deficiency virus, in association with congenital heart diseases or diseases of the left side of the heart, diseases of the respiratory system, or as an adverse reaction to several drugs) has compounded the problem of studying and managing the disease. Also, since PH is of uncommon occurrence, is diagnosed and treated by different specialists, and with different drugs, large-scale clinical trials are difficult to perform. It has thus been suggested to establish dedicated PH centers where all the patients of PH in a region are managed by skilled and experienced manpower, thereby improving patient outcomes and at the same time, also enabling better research and data collection (2). Keeping in mind the same objective, it has been suggested that clinical databases be formed wherever such centers are established (3).As has been the case with other rare and deadly diseases, the evidence on which patient care in PH has been based has rested on clinical judgment, experience of experts closely associated with the patients of PH, and assiduous collection of epidemiological and clinical information in the form of registries. The first and most important such registry in PH was the one started in the United States in 1981 – the National Institutes of Health registry (4). It not only provided precious epidemiological and clinical data, but also highlighted the poor survival rate (3-year probability of 50%) associated with the prevalent treatment in those times (5). This data paved the way for aggressive evaluation and management of PH, as a result of which some clinical trials were performed with new drugs. New insights into the pathophysiology in subsequent years have further changed the picture of this intriguing disorder. The need for conducting studies and compiling data is much greater now than it was in the 1980s because the current classification of PH is much more complex, and essential information on incidence, prevalence, natural history, and prognosis of PH in the light of current therapies is still lacking. To this effect, there have been some registries formed in different parts of the world in different subgroups (6–10). India is the largest country of south-east Asia. There is a need to study PH in Indian scenario in view of several unique characteristics like high prevalence of certain diseases (as has been well demonstrated in other chronic diseases), availability and cost of drugs, meager health resources, attitudes and cultural beliefs of the people which are quite different from the western population. We therefore sought to form a PH registry at our center to study the epidemiology, clinical profile, natural course of the disease, and response to currently available drug therapies in the country. The present report describes epidemiological data and clinical characteristics of the first 57 patients enrolled in the registry.
Methods
Ours is a single-center observational registry designed to study the demographic profile and clinical course of the patients of PH in the light of current therapies available in India. The first patient was enrolled in September 2010 and the enrollment will continue for a minimum period of 5 years.
All patients referred to Medanta PH clinic, diagnosed to have PH by right heart catheterization (RHC) (mean pulmonary artery pressure >25 mmHg), are included in the registry, irrespective of the type of PH. Those patients who refuse consent for RHC or in whom RHC is not performed but have high pulmonary artery systolic pressure (PASP >50 mmHg) on echocardiography and are clinically diagnosed to have PH according to the investigators’ judgment based on generally accepted definitions and criteria are also included. The patients not meeting above criteria are not included. In addition, the patients who have transient or acute elevations in PASP are also excluded from the registry.
After informed consent, data is obtained from the patients using a predesigned proforma and confidentiality maintained by assigning abbreviations. Baseline characteristics are obtained based on detailed history and clinical examination including eliciting typical symptoms and signs. All the investigational reports and drugs being prescribed are recorded. Exercise capacity is then measured using 6-minute walk test along with oxygen saturation at rest and immediately after 6-minute walk. Relevant investigations like blood examination, chest X-ray, comprehensive echocardiogram, pulmonary function test with diffusion capacity of carbon monoxide, computed tomographic scan of chest, RHC, etc., are performed as required to establish the diagnosis (Table 1).
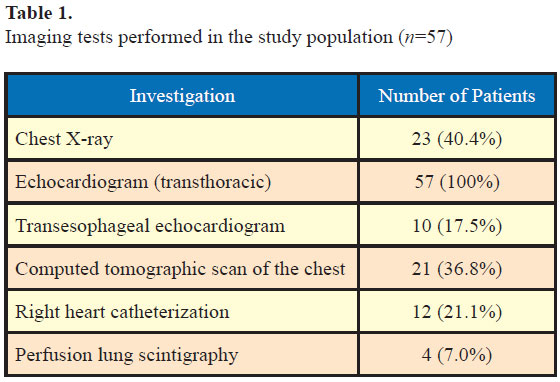
In addition, 14 patients (24.6%) also underwent pulmonary-function test by spirometry.
After initial enrolment, the patients are initiated on appropriate therapy and are followed up every 3–6 months. During each visit, relevant clinical examination along with 6-minute walk test and oxygen saturation measurement is performed. Any worsening of symptoms, development of new signs and symptoms, change in medications, development of side-effects of medications and major clinical events (balloon atrial septostomy, heart lung transplantation, etc.) are noted. Echocardiography is repeated at least once every 6 months and earlier if required. RHC and other investigations are repeated as appropriate, particularly if the patient deteriorates at any time during the follow-up. In addition to the regular hospital visits, some investigational data will be obtained on the web also by email. Each patient is scheduled to be followed for at least 5 years.
The registry has been approved by the institutional review board.
Results
We present here the baseline epidemiological and clinical data of the first 57 patients enrolled till March 2012. Out of these 57 patients, 12 were diagnosed to have PH based on RHC and the rest 45 were diagnosed on the basis of echocardiographic and clinical findings.
Demographic characteristics (Table 2)
.jpg)
In more than half of the patients (32 of 55, 58.2%), the diagnosis of PH was established during the initial month of symptom onset itself (median delay in diagnosis from the symptom onset – 1 month, interquartile range 1–33 months). However, delays of 1–5 years or even longer were not uncommon (25.5% and 10.1%, respectively). The longest interval between symptom onset and the diagnosis of PH was 20 years.
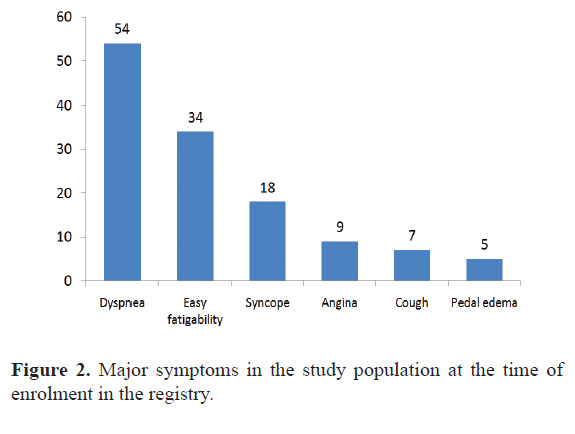
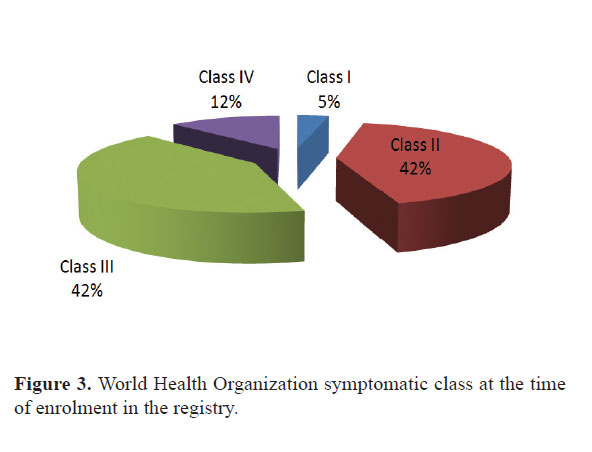
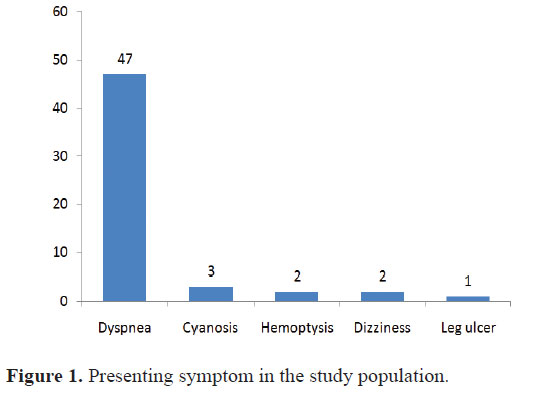
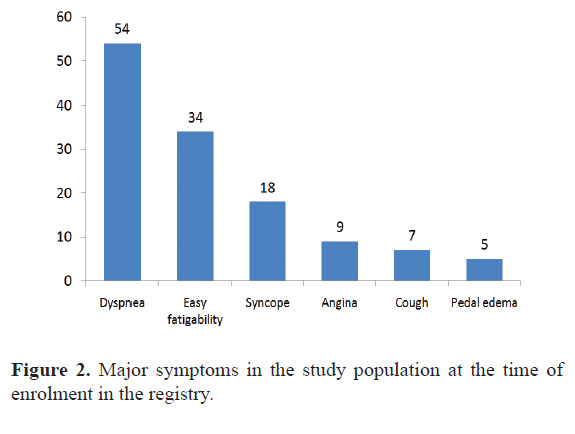
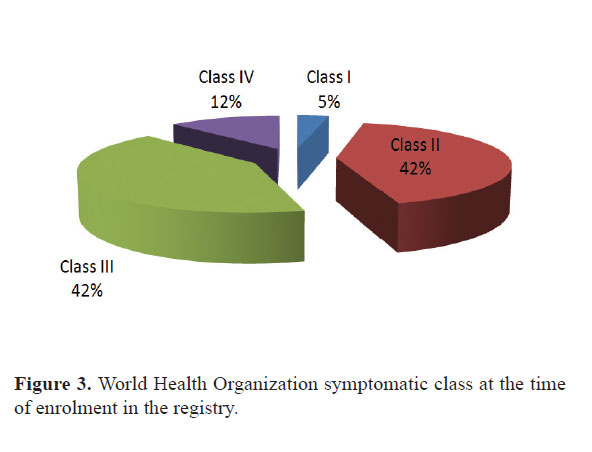
At the time of enrolment in the registry, dyspnea was again the commonest symptom (94.7%). Easy fatigability (59.6%), syncope (31.6%), angina (15.8%), cough (12.3%), pedal edema (8.8%), and epistaxis (8.8%) were other common symptoms (Fig. 2). Seven of the 18 patients with syncope had had more than one such episode. Most of the patients were in the World Health Organization functional class II or III at presentation (42% each) and only 12% were in class IV (Fig. 3).
Results
We present here the baseline epidemiological and clinical data of the first 57 patients enrolled till March 2012. Out of these 57 patients, 12 were diagnosed to have PH based on RHC and the rest 45 were diagnosed on the basis of echocardiographic and clinical findings.
Demographic characteristics (Table 2)
.jpg)
* All values are in mean ± S.D. for continuous variables and actual value with percentage in parentheses for categorical variables.
The mean age of the study population was 35.6 ± 14.3 years and almost half of the patients (49.1%) were males. There mean age of the male patients was 34.3 ± 12.2 years and of the female patients was 36.8 ± 16.1 years (p = NS). Two-thirds of all the patients were married. Majority of the patients (73.2%) were able to lead an independent life whereas 12 patients (21.4%) were dependent on others and 3 patients (5.4%) required assistance for their daily-life activities.
Among female patients, majority were housewives (19 of 29, 65.5%), 7 (24.1%) were students, and the remaining 3 (10.3%) were teachers by profession. In contrast, among the male patients majority (19 of 28, 67.9%) were vocationally active and were involved in different occupations.
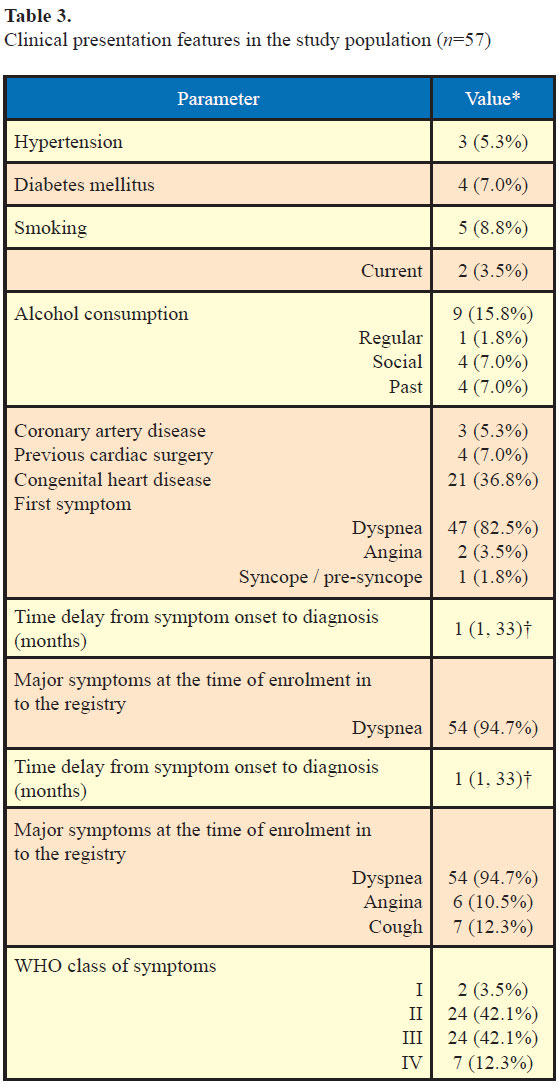
Clinical presentation (Table 3)
The mean age of the study population was 35.6 ± 14.3 years and almost half of the patients (49.1%) were males. There mean age of the male patients was 34.3 ± 12.2 years and of the female patients was 36.8 ± 16.1 years (p = NS). Two-thirds of all the patients were married. Majority of the patients (73.2%) were able to lead an independent life whereas 12 patients (21.4%) were dependent on others and 3 patients (5.4%) required assistance for their daily-life activities.
Among female patients, majority were housewives (19 of 29, 65.5%), 7 (24.1%) were students, and the remaining 3 (10.3%) were teachers by profession. In contrast, among the male patients majority (19 of 28, 67.9%) were vocationally active and were involved in different occupations.
Clinical presentation (Table 3)
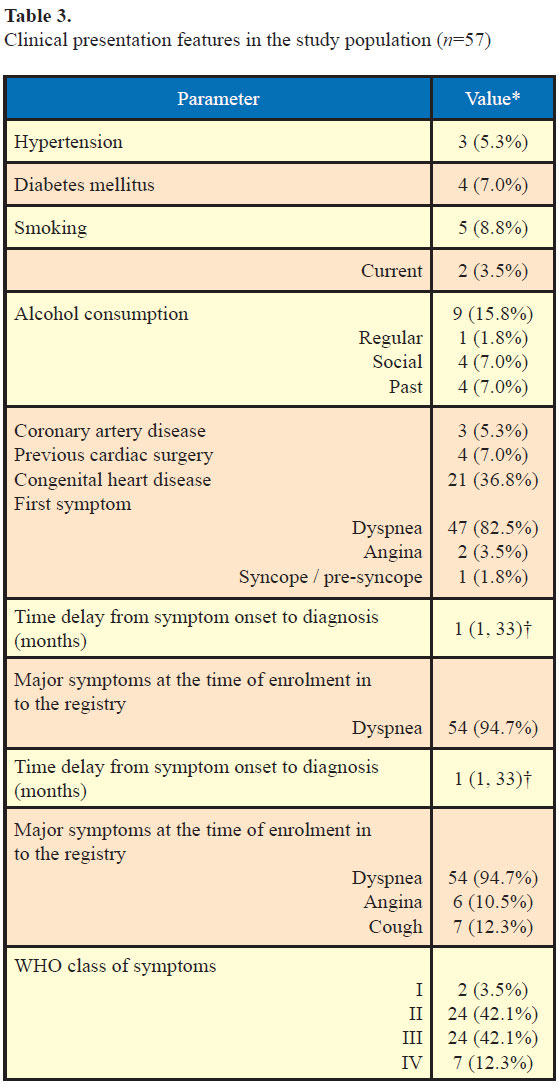
* All values are in mean ± S.D. for continuous variables and actual value with percentage in parentheses for categorical variables.
†Median (interquartile range).
WHO-World Health Organization
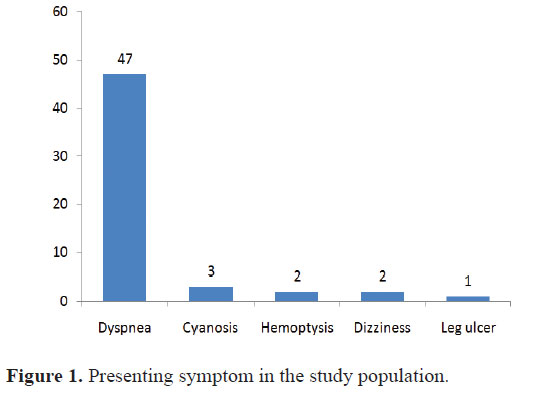
Dyspnea was the presenting symptom in the overwhelming majority of the patients (47 patients, 82.5%). Only few patients presented with other symptoms such as angina (2), cyanosis (3), hemoptysis (2), and dizziness (1) (Fig. 1). One patient was diagnosed to have chronic PH during an episode of pulmonary embolism whereas another patient was diagnosed to have PH during pregnancy.
In more than half of the patients (32 of 55, 58.2%), the diagnosis of PH was established during the initial month of symptom onset itself (median delay in diagnosis from the symptom onset – 1 month, interquartile range 1–33 months). However, delays of 1–5 years or even longer were not uncommon (25.5% and 10.1%, respectively). The longest interval between symptom onset and the diagnosis of PH was 20 years.
At the time of enrolment in the registry, dyspnea was again the commonest symptom (94.7%). Easy fatigability (59.6%), syncope (31.6%), angina (15.8%), cough (12.3%), pedal edema (8.8%), and epistaxis (8.8%) were other common symptoms (Fig. 2). Seven of the 18 patients with syncope had had more than one such episode. Most of the patients were in the World Health Organization functional class II or III at presentation (42% each) and only 12% were in class IV (Fig. 3).
Although a major congenital heart disease was present in 36.8% patients, other comorbidities were uncommon. Hypertension and diabetes were present only in three and four patients, respectively, and only five patients were current or past smokers. Alcohol consumption was also uncommon with 48 patients (84.2%) being teetotalers. Similarly, coronary artery disease was also rare in the study population (5.3%). However, four patients had undergone cardiovascular surgery in past (two valve replacements, one atrial septal defect closure, and one coronary artery bypass surgery).
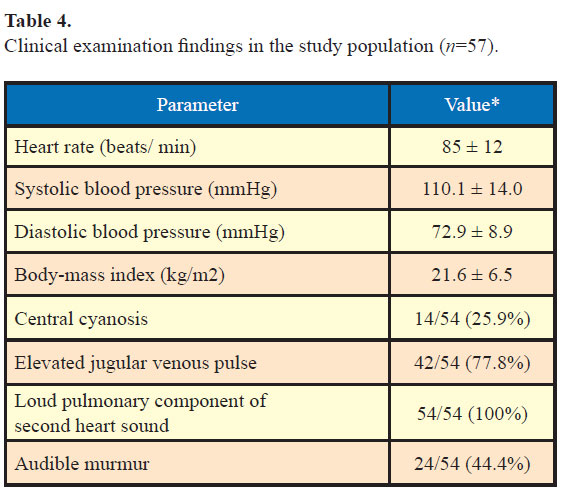
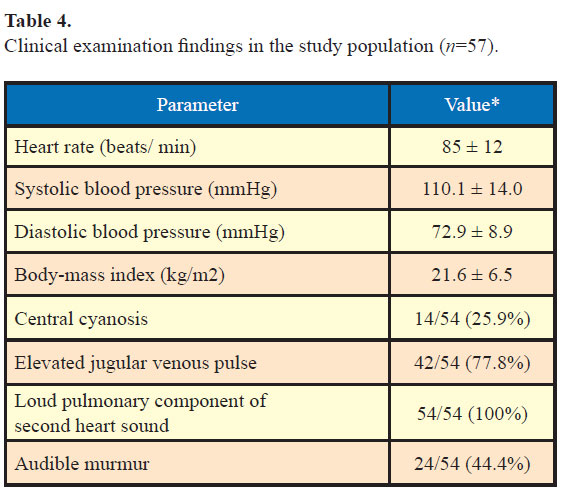
Clinical examination findings (Table 4)
The complete clinical examination findings were available for 54 patients. The average heart rate at rest was 72.9 ± 8.9 beats/min and the average systolic and diastolic blood pressure were 110.1 ± 14.0 mmHg and 85 ± 12 mmHg, respectively. Clinically apparent central cyanosis was present in 14 patients (25.9%). Jugular venous pressure was elevated in 77.8% patients. On precordial examination, all the patients had loud pulmonary component of the second heart sound and 44.4% patients had an audible murmur (mostly tricuspid regurgitation).
* All values are in mean ± S.D. for continuous variables and actual value with percentage in parentheses for categorical variables.
* All values are in mean ± S.D. for continuous variables and actual value with percentage in parentheses for categorical variables.
Of the 57 subjects, 12 could not walk at all. Hence, the 6-minute walk distance could be measured in the remaining 45 patients only. The mean distance walked by them was 291.7 ± 122.4 m. Immediately following the 6-minute walk, SaO2 remained unchanged (or decreased by <5%) in 25 patients (55.6%) but appreciably decreased (>5% absolute reduction) in 11 patients (24.4%).
Clinical examination findings (Table 4)
The complete clinical examination findings were available for 54 patients. The average heart rate at rest was 72.9 ± 8.9 beats/min and the average systolic and diastolic blood pressure were 110.1 ± 14.0 mmHg and 85 ± 12 mmHg, respectively. Clinically apparent central cyanosis was present in 14 patients (25.9%). Jugular venous pressure was elevated in 77.8% patients. On precordial examination, all the patients had loud pulmonary component of the second heart sound and 44.4% patients had an audible murmur (mostly tricuspid regurgitation).
* All values are in mean ± S.D. for continuous variables and actual value with percentage in parentheses for categorical variables.
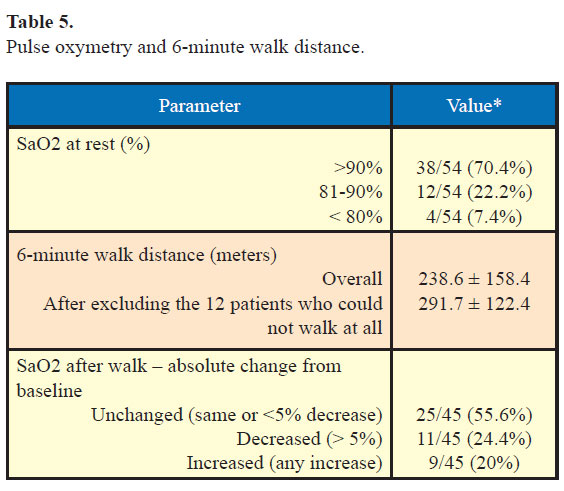
Pulse oxymetry and 6-minute walk distance (Table 5)
The resting pulse oxymetry data was available for 54 patients. Of these, 38 patients (70.4%) had SaO2 >90%,12 (22.2%) had SaO2 81–90%, and 4 (7.4%) had SaO2 <80%.
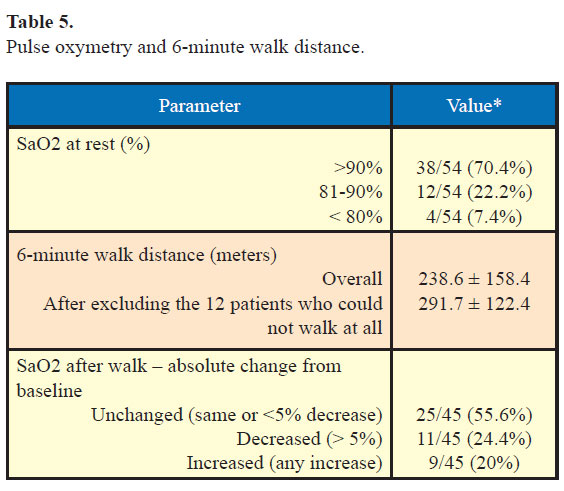
* All values are in mean ± S.D. for continuous variables and actual value with percentage in parentheses for categorical variables.
Of the 57 subjects, 12 could not walk at all. Hence, the 6-minute walk distance could be measured in the remaining 45 patients only. The mean distance walked by them was 291.7 ± 122.4 m. Immediately following the 6-minute walk, SaO2 remained unchanged (or decreased by <5%) in 25 patients (55.6%) but appreciably decreased (>5% absolute reduction) in 11 patients (24.4%).
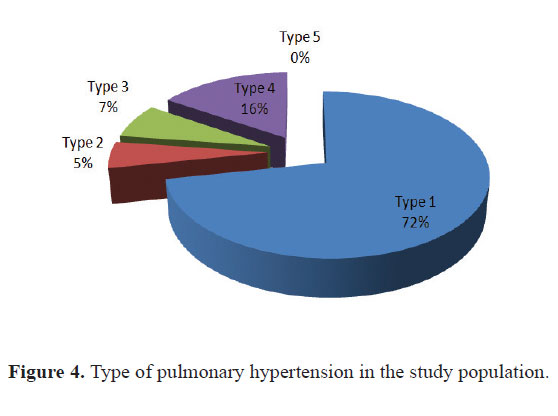
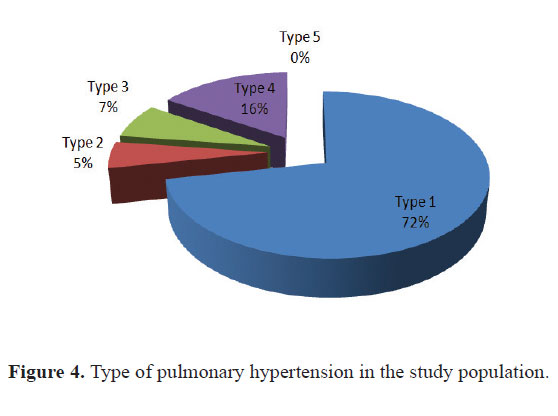
PH types (Fig. 4)
Type I was the commonest (72%) and the type II was the second most common (16%) form of PH in our registry. Type III and IV were less common (5% and 7%, respectively) whereas no patient had type V PH. Among patients with type I PH, the largest chunk was contributed by idiopathic PH followed by patients with congenital heart disease (36.8%). There was no patient with familial PH.
Discussion
A This is the largest ever PH registry data from India and yields an insight into the epidemiological characteristics of the patients of PH.
The mean age of the patients (35.6 ± 14.3 years) is quite similar to that in the NIH registry data (4). However, the male–female ratio is almost equal in our data whereas it is generally been shown to have a female preponderance in almost all previous registries – male–female ratio 1.7 in the NIH and 1.9 in the French registry data (11). This may represent a social trend of under diagnosis and treatment in women in this part of the world as is common in other diseases. Another interesting finding is the marital status of the majority of patients (two-third). This can have wide ranging social implications since pregnancy is contraindicated in women with PH. Also, since India is a male-dominated society, the prognosis of the disease can destroy the families dependent on males for their support. Most of the patients in our study were independent and males were vocationally active, which is a good sign since it means that the disease has been diagnosed before the onset of debilitating symptoms. The average time to diagnosis from symptom onset has been less than a month which is quite remarkable. Late diagnosis has been the bane of PH as has been reflected in the NIH, French, and other registries (4,11). Our data probably is representative of the fact that most patients were referred to a center equipped with echocardiography and were mainly living in an urban setting. However, the detection of PH after 20 years of symptom onset in one patient and delay of 1–5 years in 25.5% of patients highlight the fact that awareness about the disease is still lacking even in urban areas and late detection continues to be a threat for optimum management of PH.
Maximum patients (42% each) were in WHO class II and III at the time of diagnosis. This is also an important factor since WHO class remains a vital prognostic factor, with earlier detection resulting in better management and survival. Delayed detection or late presentation has been a finding in most previous registries. In the French registry, for example, 75% patients were in class III or IV and 24% were in class II (11). Dyspnea was the commonest presenting symptom in our patients and this finding is quite consistent with all other registry data. Other clinical findings were consistent with underlying clinical condition. Central cyanosis was present in 25.5% of the patients while loud second heart sound (100%) and audible murmur of TR (44.4%) were other common clinical signs. The association of other clinical conditions like hypertension, diabetes, and obesity was quite low, probably owing to the younger age of the patients.
The 6-minute walk test is a submaximal exercise test that can be safely performed by patients incapable of tolerating maximal exercise testing (12). It is straightforward, reproducible, and does not require any equipment. The distance walked in 6 minutes has a strong independent association with mortality and correlates with functional class (11,13). The mean overall 6-minute walk distance in our patients has been 238.6 m, which is consistent with the functional class II and III in most patients. A 6-minute walk distance of less than 165 m has been considered to be a poor prognosticator in the recently proposed REVEAL (Registry to EValuate Early AND Long-term PAH disease management) risk score (14). Oxygen saturation at rest and after 6-minute walk is also a useful marker of functional capacity and was assessed in our patients. In most (70.4%) of our patients, oxygen saturation was greater than 90% at rest and in more than half of them, it remained same or reduced by less than 5%. In about a quarter of the patients, oxygen saturation measured by pulse oxymetry reduced by more than 5%. These findings are also consistent with the fact that most of the patients were in functional class II and III.
The commonest type of PH in our data was type I or pulmonary arterial hypertension. The largest share in this was from congenital heart disease and idiopathic varieties. There has been no patient of familial PAH. This is quite understandable considering the relative rarity of the condition, cost, availability of genetic testing, and our reliance on history taking for the diagnosis. The representation from connective tissue disorders is also less than expected, probably due to lack of utilization of echocardiography for screening, problems related to interspecialty referral, lack of awareness among rheumatologists, or a combination of these factors. Also, there has been no case of PH due to the use of appetite suppressant drugs (fenfluramine derivatives), which is quite different from the data from the west. This probably is due to the lack of availability, and consequently limited used, of such drugs in India. The absence of patients of type V PH (miscellaneous causes like sarcoidosis, histiocytosis X, etc.) is probably due to rarity of these conditions and underdetection due to lack of knowledge about the association with PH in these conditions.
Discussion
A This is the largest ever PH registry data from India and yields an insight into the epidemiological characteristics of the patients of PH.
The mean age of the patients (35.6 ± 14.3 years) is quite similar to that in the NIH registry data (4). However, the male–female ratio is almost equal in our data whereas it is generally been shown to have a female preponderance in almost all previous registries – male–female ratio 1.7 in the NIH and 1.9 in the French registry data (11). This may represent a social trend of under diagnosis and treatment in women in this part of the world as is common in other diseases. Another interesting finding is the marital status of the majority of patients (two-third). This can have wide ranging social implications since pregnancy is contraindicated in women with PH. Also, since India is a male-dominated society, the prognosis of the disease can destroy the families dependent on males for their support. Most of the patients in our study were independent and males were vocationally active, which is a good sign since it means that the disease has been diagnosed before the onset of debilitating symptoms. The average time to diagnosis from symptom onset has been less than a month which is quite remarkable. Late diagnosis has been the bane of PH as has been reflected in the NIH, French, and other registries (4,11). Our data probably is representative of the fact that most patients were referred to a center equipped with echocardiography and were mainly living in an urban setting. However, the detection of PH after 20 years of symptom onset in one patient and delay of 1–5 years in 25.5% of patients highlight the fact that awareness about the disease is still lacking even in urban areas and late detection continues to be a threat for optimum management of PH.
Maximum patients (42% each) were in WHO class II and III at the time of diagnosis. This is also an important factor since WHO class remains a vital prognostic factor, with earlier detection resulting in better management and survival. Delayed detection or late presentation has been a finding in most previous registries. In the French registry, for example, 75% patients were in class III or IV and 24% were in class II (11). Dyspnea was the commonest presenting symptom in our patients and this finding is quite consistent with all other registry data. Other clinical findings were consistent with underlying clinical condition. Central cyanosis was present in 25.5% of the patients while loud second heart sound (100%) and audible murmur of TR (44.4%) were other common clinical signs. The association of other clinical conditions like hypertension, diabetes, and obesity was quite low, probably owing to the younger age of the patients.
The 6-minute walk test is a submaximal exercise test that can be safely performed by patients incapable of tolerating maximal exercise testing (12). It is straightforward, reproducible, and does not require any equipment. The distance walked in 6 minutes has a strong independent association with mortality and correlates with functional class (11,13). The mean overall 6-minute walk distance in our patients has been 238.6 m, which is consistent with the functional class II and III in most patients. A 6-minute walk distance of less than 165 m has been considered to be a poor prognosticator in the recently proposed REVEAL (Registry to EValuate Early AND Long-term PAH disease management) risk score (14). Oxygen saturation at rest and after 6-minute walk is also a useful marker of functional capacity and was assessed in our patients. In most (70.4%) of our patients, oxygen saturation was greater than 90% at rest and in more than half of them, it remained same or reduced by less than 5%. In about a quarter of the patients, oxygen saturation measured by pulse oxymetry reduced by more than 5%. These findings are also consistent with the fact that most of the patients were in functional class II and III.
The commonest type of PH in our data was type I or pulmonary arterial hypertension. The largest share in this was from congenital heart disease and idiopathic varieties. There has been no patient of familial PAH. This is quite understandable considering the relative rarity of the condition, cost, availability of genetic testing, and our reliance on history taking for the diagnosis. The representation from connective tissue disorders is also less than expected, probably due to lack of utilization of echocardiography for screening, problems related to interspecialty referral, lack of awareness among rheumatologists, or a combination of these factors. Also, there has been no case of PH due to the use of appetite suppressant drugs (fenfluramine derivatives), which is quite different from the data from the west. This probably is due to the lack of availability, and consequently limited used, of such drugs in India. The absence of patients of type V PH (miscellaneous causes like sarcoidosis, histiocytosis X, etc.) is probably due to rarity of these conditions and underdetection due to lack of knowledge about the association with PH in these conditions.
Limitations
There are some limitations with our registry that need consideration. We have collected the data of all patients of PH being referred to us from different parts of the country, though the majority of patients are from northern part of the country. Thus, we can by no means claim that this data is representative of the prevalence of PH and its different subtypes in the region. Some patients have opted to be kept out of the registry yet continue the treatment at our PH center. Further, it is likely that the patients with functional class I and II are underrepresented since they are less likely to be diagnosed at this stage.
The standard definition of PH is based on RHC. All the patients were explained about the need of RHC but most patients did not opt for it on account of reasons of cost, invasive nature, travel involved to a higher center, risk of the procedure, etc. A broad definition of PH has been Journal of Clinical and Preventive Cardiology April 2012 | Number 2 Mehrotra et al [ 57 ] thus kept to include all patients of PH as has been done in some of the registries in the past [SOPHIA (Surveillance of Pulmonary Hypertension in America) registry and the Chinese registry] (6,8).
The standard definition of PH is based on RHC. All the patients were explained about the need of RHC but most patients did not opt for it on account of reasons of cost, invasive nature, travel involved to a higher center, risk of the procedure, etc. A broad definition of PH has been Journal of Clinical and Preventive Cardiology April 2012 | Number 2 Mehrotra et al [ 57 ] thus kept to include all patients of PH as has been done in some of the registries in the past [SOPHIA (Surveillance of Pulmonary Hypertension in America) registry and the Chinese registry] (6,8).
Conclusions
This registry provides novel information on the clinical and epidemiological features of all types of PH in the subcontinent. This registry highlights some unique characteristics of PH in the light of current era of awareness and treatment. Some of the findings are quite similar to the western data but some interesting observations have also emerged. There remains a need to spread awareness about PH among the physicians and specialists since it occurs in association with myriad diseases. The diagnosis is still made quite late in a substantial number of patients which hampers the optimum management even in the current era of effective drug therapy. The ongoing registry will also throw light on the response to various drugs and survival in the light of these drugs. There is, however, a definite need to form a large-scale registry in the subcontinent with uniform diagnostic criteria to better understand the unique demographics of this uncommon but devastating cardiovascular disease.
Acknowledgement
We sincerely thank Mr. Arun Rawat and Ms Sugy Samuel, clinical research coordinators for the study, for their immense help in data collection and compilation.
Funding
No external source of funding
Conflict of interest
None
References
References
- R Romberg E. Ueber slerose der lungenarterien. Deutsch Arch Klin Med. 1891; 48:197.
- Pulmonary hypertension in clinical practice in the UK and Ireland. National pulmonary centres of the UK and Ireland. Thorax. 2008; 63(Suppl II):ii1–ii41.
- Michelakis ED, Wilkins MR, Rabinovitch M. Pulmonary vascular diseases. Emerging concepts and translational priorities in pulmonary arterial hypertension. Circulation. 2008; 118:1486–95.
- Rich S, Dantzker DR, Ayres SM, Bergofsky EH, Brundage BH, Detre KM, Fishman AP, Goldring RM, Groves BM, Koerner SK et al. Primary pulmonary hypertension: a national prospective study. Ann Intern Med.1987; 107(2):216–23.
- D’Alonzo GE, Barst RJ, Ayres SM, Bergofsky EH, Brundage BH, Detre KM, Fishman AP, Goldring RM, Groves BM, Kernis JT et al. Survival in patients with primary pulmonary hypertension: results from a national prospective study. Ann Intern Med. 1991; 115(5):343–9.
- Jing ZC, Xu XQ, Han ZY, Wu Y, Deng KW, Wang H, Wang ZW, Cheng XS, Xu B, Hu SS, Hui RT, Yang YJ.. Registry and survival study in Chinese patients with idiopathic and familial pulmonary arterial hypertension. Chest. 2007; 132(2):373–9.
- Rich S, Rubin L, Walker AM, Schneeweiss S, Abenhaim L. Anorexigens and pulmonary hypertension in the United States: results from the surveillance of North American pulmonary hypertension. Chest. 2000; 117(3):870–4.
- Walker AM, Langleben D, Korelitz JJ, Rich S, Rubin LJ, Strom BL, Gonin R, Keast S, Badesch D, Barst RJ, Bourge RC, Channick R, Frost A, Gaine S, McGoon M, McLaughlin V, Murali S, Oudiz RJ, Robbins IM, Tapson V, Abenhaim L, Constantine G.. Temporal trends and drug exposures in pulmonary hypertension: an American experience. Am Heart J. 2006; 152(3):521–6.
- Stricker H, Domenighetti G, Popov W, Speich R, Nicod L, Aubert JD, Solèr M; Swiss Group for Severe Pulmonary Hypertension Severe pulmonary hypertension: data from the Swiss Registry. Swiss Med Wkly. 2001; 131(23–24):346–50.
- McGoon MD, Krichman A, Farber HW, Barst RJ, Raskob GE, Liou TG, Miller DP, Feldkircher K, Giles S.Design of the REVEAL registry for US patients with pulmonary arterial hypertension. Mayo Clin Proc. 2008; 83 (8):923–31.
- Humbert M, Sitbon O, Chaouat A, Bertocchi M, Habib G, Gressin V, Yaici A, Weitzenblum E, Cordier JF, Chabot F, Dromer C, Pison C, Reynaud-Gaubert M, Haloun A, Laurent M, Hachulla E, Simonneau G.. Pulmonary arterial hypertension in France: results from a national registry. Am J Respir Crit Care Med. 2006; 173(9):1023–30.
- Miyamoto S, Nagaya N, Satoh T, Kyotani S, Sakamaki F, Fujita M, Nakanishi N, Miyatake K.. Clinical correlates and prognostic significance of six-minute walk test in patients with primary pulmonary hypertension: comparison with cardiopulmonary exercise testing. Am J Respir Crit Care Med. 2000; 161:487–92.
- Sitbon O, Humbert M, Nunes H, Parent F, Garcia G, Hervé P, Rainisio M, Simonneau G.. Long-term intravenous epoprostenol infusion in primary pulmonary hypertension: prognostic factors and survival. J Am Coll Cardiol. 2002; 40:780–8.
- Benza RL, Gomberg-Maitland M, Miller DP, Frost A, Frantz RP, Foreman AJ, Badesch DB, McGoon MD.. The REVEAL registry risk score calculator in patients newly diagnosed with pulmonary arterial hypertension. Chest. 2012; 141:354–62.
- Why Publish with JCPC?
- Instructions to the Authors
- Submit Manuscript
- Advertise with Us
- Journal Scientific Committee
- Editorial Policy
Print: ISSN: 2250-3528


