The Journal of Clinical and Preventive Cardiology has moved to a new website. You are currently visiting the old
website of the journal. To access the latest content, please visit www.jcpconline.org.
Student's Page
Wide QRS Complex Tachycardia
Volume 1, Oct 2012
Kartikeya Bhargava, MD, DNB, Gurgaon, India
J Clin Prev Cardiol 2012;1(4):205-7
Wide QRS Complex Tachycardia
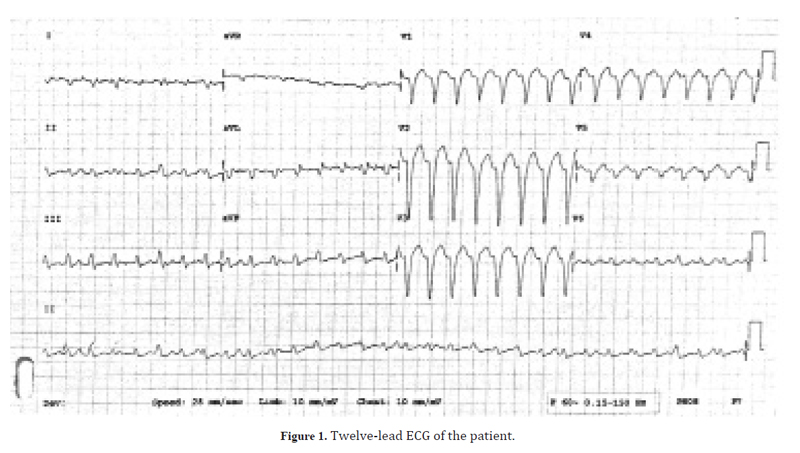
A 36-year-old lady presented with complaints of palpitations. She had history of similar complaints since past 3 months with frequent episodes that used to resolve spontaneously. There was no history of syncope or presyncope. The patient was hemodynamically stable with a blood pressure of 110/80 mmHg. The ECG recorded in the emergency room is shown in the Figure 1. An echocardiogram revealed normal structure and function of left and right ventricles. What is the ECG diagnosis?
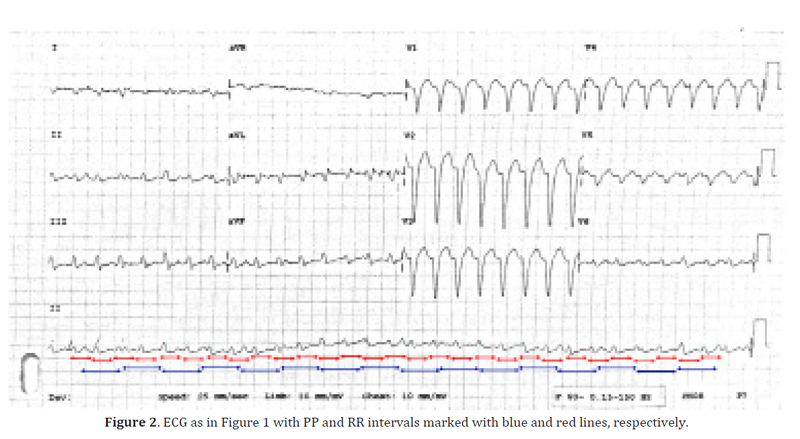
The ECG shows a regular tachycardia with ventricular rate of 188 beats per minute. The QRS is wide (140 ms) and is predominantly negative in lead V1 suggesting left bundle branch block (LBBB) type pattern. The QRS is negative in lead I and positive in lead aVF indicating right axis deviation of the QRS in the frontal plane. Careful observation reveals that the number of P-waves is much less than the number of QRS complexes; the P-waves occur at regular intervals and have no relationship with the QRS complexes indicating atrioventricular (AV) dissociation. The PP interval is shown as blue lines in Figure 2 and indicates a regular atrial rhythm with a rate of 110/min.
The QRS complexes are monomorphic, that is, of same morphology but on occasions show slightly different morphology as a result of distortion due to superimposed P-waves. All these features indicate a diagnosis of ventricular tachycardia (VT). Moreover, VT with LBBB type morphology with inferior (rightward) axis of the QRS complex suggests origin in the right ventricular outflow tract. Although, with LBBB morphology tachycardia, a QRS duration of greater than 160 ms suggests VT, relatively narrow QRS complexes in the present case suggest that the origin may be near the interventricular septum resulting in near simultaneous depolarization of the two ventricles. Thus, a final diagnosis of monomorphic VT arising from septal region of outflow tract can be made.
- Ventricular tachycardia
- Supraventricular tachycardia (SVT) with
a. Preexisting BBB
b. BBB due to aberrant conduction during SVT - Preexcited tachycardia – any SVT with antegrade conduction over an AV accessory pathway.
Although SVT with aberrancy is often thought of in the differential diagnosis of a WQRST, in clinical practice 80% of WQRSTs are ventricular in origin (2). Preexcited tachycardia is very rare and is suggested by ventricular preexcitation during sinus rhythm. SVT with BBB is seen often in the electrophysiology lab, but is fairly uncommon in clinical tachycardias. Moreover, the presence of structural heart disease in association with WQRST suggests VT as the cause in 95% of the cases. Also, a history of previous myocardial infarction is associated with very high (98%) incidence of VT as the mechanism of WQRST (2). Hence, VT should always be the initial diagnosis in a patient with WQRST unless proved otherwise.
Another misconception is that VT is hemodynamically unstable and SVT is stable. However, it is not true. VT can be stable even in severe left ventricular dysfunction and SVT on the other hand may result occasionally in hemodynamic instability and syncope.
Many criteria and algorithms (3–5) have been published to aid in the differential diagnosis of WQRST. Some of these criteria include the following:
- QRS duration. A VT results in a wide QRS complex due to sequential activation of the two ventricles. QRS duration >140 ms with right bundle branch morphology (RBBB) and >160 ms with LBBB suggests VT (3). However, a VT arising in the septum may result in a tachycardia with a shorter QRS duration. Also, SVT in patients with hyperkalemia or on amiodarone or class Ic anti-arrhythmic drugs can occur with wide QRS complexes.
- QRS axis. An abnormal QRS axis (northwest axis) suggests VT. Also, discordance of axis and morphology pattern, that is, right axis deviation with LBBB morphology and left axis deviation with RBBB morphology during tachycardia (if absent during sinus rhythm), is suggestive of VT.
- AV dissociation. AV dissociation is highly specific for a diagnosis of VT. However, 40% of WQRST do not have AV dissociation. Also, it may not be discernible in many in the surface ECG. Only 25% of WQRST have discernible AV dissociation. Capture and fusion beats also occur in the background of AV dissociation and are highly suggestive of VT. More QRS complexes than P-waves (VA block) are also very specific for VT.
- Baseline ECG with BBB. A WQRST with BBB with morphology identical to that during sinus rhythm is indicative of SVT with the exception of bundle branch reentry VT. Thus, the fact that BBB is present during sinus rhythm is of great help in the diagnosis. Also, if a tachycardia has a QRS that is narrower than during sinus rhythm, it is also diagnostic of VT.
- Morphology criteria. Various morphology criteria that are different for LBBB and RBBB morphology patterns have been described but are difficult to memorize (4,5). It is suffice to say if a tachycardia resembles a typical LBBB or RBBB pattern, it is more likely to be SVT and if the morphology is atypical, it is more likely to be VT.
One should remember that all the criteria that are used to differentiate VT from SVT with BBB are useful if they are positive but do not rule out VT if they are negative. For example, the presence of AV dissociation during a WQRST suggests a diagnosis of VT but its absence does not rule out VT.
To summarize, the diagnosis of VT in the present case was suggested by WQRST itself, presence of LBBB morphology with right axis deviation (axis-morphology discordant pattern), more QRS complexes than P-waves, and AV dissociation.
Conflicts of Interest
None.
Source of Funding
None.
References
- Wellens HJJ. Ventricular tachycardia: diagnosis of broad QRS complex tachycardia. Heart. 2001; 86:576–85.
- Akhtar M, Shenasa M, Jazayeri M, Caceres J, Tchou PJ. Wide QRS complex tachycardia. Reappraisal of a common clinical problem. Ann Intern Med. 1988; 109:905–12.
- Wellens HJJ, Bar FWHM, Lie KI. The value of the electrocardiogram in the differential diagnosis of a tachycardia with a widened QRS complex. Am J Med. 1978; 64:27–33.
- Brugada P, Brugada J, Mont L, Smeets J, Andries EW. A new approach to the differential diagnosis of a regular tachycardia with a wide QRS complex. Circulation. 1991; 83:1649–59.
- Kindwall E, Brown J, Josephson ME. Electrocardiographic criteria for ventricular tachycardia in wide QRS complex left bundle-branch block morphology tachycardia. Am J Cardiol. 1988; 61:1279–83.
- Why Publish with JCPC?
- Instructions to the Authors
- Submit Manuscript
- Advertise with Us
- Journal Scientific Committee
- Editorial Policy
Print: ISSN: 2250-3528