The Journal of Clinical and Preventive Cardiology has moved to a new website. You are currently visiting the old
website of the journal. To access the latest content, please visit www.jcpconline.org.
Student's Page
Ventilatory Support
Volume 2, Jul 2013
Jeetendra Sharma MD, IFCC, Mukesh Gupta MD, DNB, Gurgaon, Haryana, India
J Clin Prev Cardiol. 2013;2(3):170-5
IntroductionVentilatory support is one of the essential and common methods of care or treatment seen in intensive care. Respiratory failure is the primary indication of ventilatory support but sometimes, hemodynamic instability, multi-organ dysfunction and unconsciousness are other indications of ventilator support. In cardiac critically ill patient, this modality plays a dual role - to support breathing and to increase cardiac performance due to cardiopulmonary interaction. To understand ventilator functioning and management, we have to understand the basic pathophysiology of respiratory failure.
Respiratory failure is of two types:
- Type 1 – Hypoxic respiratory failure
- Type 2 – Hypercarbic respiratory failure
Type 1 (Hypoxic respiratory failure) – Oxygenation impairment is the characteristic feature of type 1 respiratory failure. The oxygen content of blood decreases to a level which is life threatening. This is seen in conditions of pulmonary edema, lung collapse, lung consolidation, lung infections, lung contusion and acute respiratory distress syndrome (ARDS). The alveolar-arteriolar oxygen gradient increases very much causing ventilation perfusion mismatch. In other terms, the shunt fraction increases, which means alveoli are perfused but not ventilated.
Type 2 (Hypercarbic respiratory failure) – Ventilation impairment is the characteristic feature of type 2 respiratory failure. This can occur in conditions of comneuromuscular weaknesses (Guillian-Barre syndrome, myasthenia gravis), metabolic disorders (hypokalemia, hyperkalemia), upper airway pathologies (laryngeal edema, trauma) or chest bellows dysfunction (rib fracture, flail chest, pneumothorax, and pleural effusion). In type 2 respiratory failure, the level of CO2 increases to a point of endangering the life. There is again a mismatch of ventilation and perfusion causing increased dead space i.e., ventilation without perfusion.
Breathing can be supported non-invasively or invasively by ventilator. A ventilator is a machine that supports breathing. Functions of a ventilator are:
Your file has been successfully uploaded
A.) Type 1 respiratory failure
B.) Type 2 respiratory failure
Contraindications of NIV
Complications of NIV
Invasive Ventilation
Ventilatory Support
Breathing can be supported non-invasively or invasively by ventilator. A ventilator is a machine that supports breathing. Functions of a ventilator are:
- Provide oxygen into the lungs and helps in oxygenation
- Remove carbon dioxide from the body by lungs
- Support spontaneous breathing
- Breathing for patients who have lost all ability to breathe on their own
Non-invasive ventilation (Figure 1)
Non-invasive ventilation (NIV) refers to the administration of ventilatory support without using an invasive artificial airway (endotracheal tube or tracheostomy tube). NIV is delivered via face mask, nasal mask or helmet. The clinical efficacy of NIV depends upon the mode used, and the nature and severity of the underlying respiratory disorder. NIV can substantially reduce the need for endotracheal intubation and invasive mechanical ventilation. In selected patients, the benefits of NIV include decreased rates of adverse events associated with invasive mechanical ventilation, shorter ICU and hospital stay, and lower mortality rates.
Your file has been successfully uploaded
A.) Type 1 respiratory failure
- Cardiogenic pulmonary edema
- Pneumonia
- Mild ARDS
- Post thoracic surgery
- Post abdominal surgery
- Post cardiac surgery
B.) Type 2 respiratory failure
- COPD
- Acute asthma
- Obstructive sleep apnea
- Neuromuscular weaknesses
- Chest wall deformity
- Cystic fibrosis
Contraindications of NIV
- Respiratory arrest
- Severe hypoxia
- Inability to protect airway (unconscious, stroke, bulbar palsy)
- Copious respiratory secretions
- Severe hemodynamic instability
- Facial abnormality (facial trauma, facial burn)
- Persistent vomiting
- Post-operative gastrointestinal surgery
- Respiratory secretions
Complications of NIV
- Delay in intubation
- Discomfort
- Claustrophobia
- Facial and nasal bridge pressure sore
- Ocular abrasions
- Gastric distension
- Nasal congestion
- Oro-nasal dryness
- Pneumothorax (in bullous lung disease)
- Aspiration pneumonia
- Hypotension
Invasive Ventilation
Invasive mechanical ventilation (Figure 2 and 3) is achieved through means of endotracheal tube or tracheostomy tube.
.jpg)

[A] According to pre-set delivery of breath
[B] According to triggering
Broadly there are two major modes of ventilation:
a) Assist control ventilation: AC mode is generally the initial mode of ventilation. In this, the breath is delivered either volume cycled (volume pre-set) or time cycled (pressure pre-set). A predetermined tidal volume or a predetermined applied pressure for a fixed duration is delivered at a pre-set minimal rate. The patient receives a minimum number of breaths, pre-determined on the ventilator. These breaths may be synchronized to patient’s inspiratory effort if present, and there are additional breaths to pre-set minimum rate. Therefore, the number of breaths may actually increase if there is increased number of patient’s inspiratory efforts, causing hyperventilation.
b) Synchronized intermittent mandatory ventilation: In SIMV, mandatory breaths, as pre-set on ventilator are delivered along with spontaneous breaths interspersed between mandatory breaths. These breaths again can be volume cycled or time cycled. The mandatory breaths are synchronized with patient’s spontaneous breaths, which help in better patient ventilator interaction. This mode is utilized for weaning process.
c) Pressure support ventilation: There are no mandatory breaths but all breaths are spontaneous (triggered by patient). Each spontaneous breath is augmented with positive pressure set on the ventilator. These breaths are flow cycled and help in decreasing work of breathing. This mode is utilized for weaning purpose.
Ventilator Setting
(b) Minute Volume – Minute volume is a product of tidal volume and respiratory rate. It is adjusted to keep partial pressure of carbon dioxide in arterial blood (PaCO2) within acceptable limits (35–45 mmHg).
(c) Inspiratory expiratory ratio (I:E) – It is ratio of duration of inspiration to expiration. Usually this ratio is set 1:2 for normal ventilation. A ratio more than 1:1 and rapid inspiratory flow rate minimize the hemodynamic effect of positive pressure ventilation and improves oxygenation but increases PaCO2. An I:E ratio of 2:1 – 4:1 is known as inverse ratio ventilation (IRV). In IRV, the slow, long inspiration ensures distribution of ventilation to alveoli, which are slow to open up. IRV may cause dynamic hyperinflation (intrinsic PEEP) and hypercapnea.
(d) Positive end – expiratory pressure (PEEP) - This exists when airway pressure gradient is greater than ambient pressure just before the next inspiration. It is an integral part of mechanical ventilation in the management of acute alveolar pathology such as ARDS. About 4-5 cm H2O is a physiological PEEP, higher than this PEEP is indicated when it is not possible to maintain acceptable PaO2 (>60 mmHg) at FiO2 of 0.5-0.6. PEEP improves gas exchange and oxygenation at the same FiO2. PEEP also helps in recruitment of collapsed alveoli and keeps them open for ventilation, thereby minimizing the risk of shear force injury to alveoli.
.jpg)

Terminology
Description of ventilatory support and ventilator frequently uses few terms:
- Triggering - Conversion of patient’s expiration to inspiration
- Cycling - Conversion of patient’s inspiration to expiration
- Limit – Pre-set variable for inspiratory phase
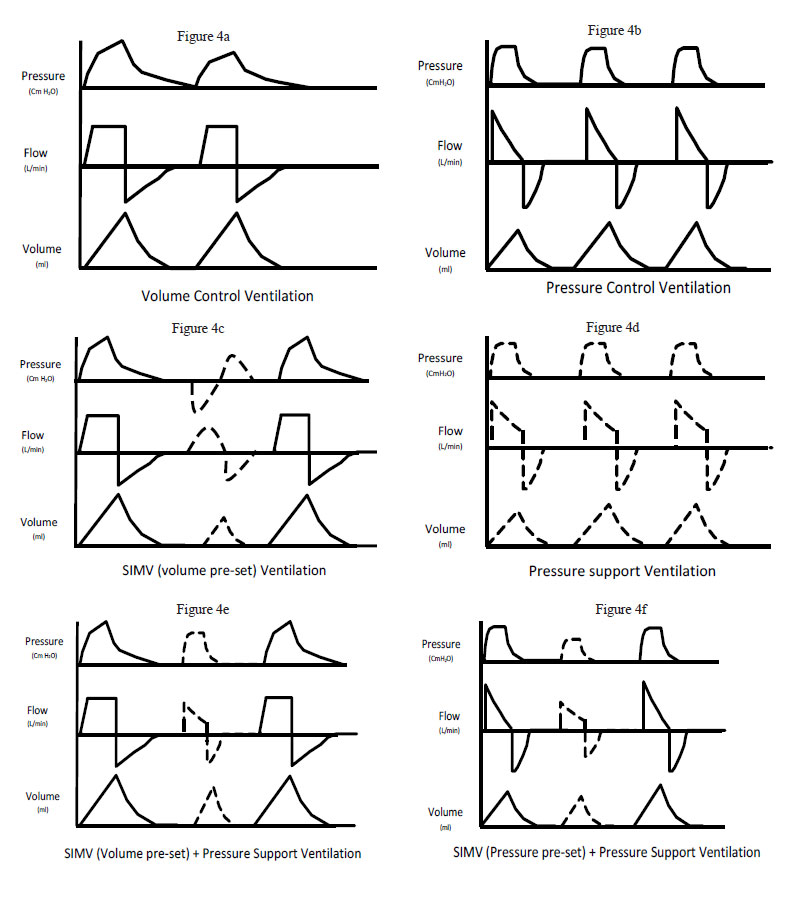
Classification of Different Modes of Ventilation (Figure 4 a-f)
[A] According to pre-set delivery of breath
- Volume pre-set (e.g. volume control, synchronized intermittent mandatory ventilation [SIMV] volume control, volume support)
- Pressure pre-set (e.g. pressure control, SIMV pressure control, pressure support)
- Dual – Pressure regulated volume pre-set
[B] According to triggering
- Control mode - No triggering by patient, time triggered, either volume pre-set (flow cycled) or pressure pre-set (time cycled) e.g. volume control, pressure control
- Assist Control (AC) – Triggered by patient as well by time, either volume pre-set (flow cycled) or pressure pre-set (time cycled) e.g. volume assist control, pressure assist control
- Partial Ventilation modes – These modes are not only required for triggering by patients but these actually participate during inspiration. Following are examples of partial ventilation:
- Pressure Support Ventilation (PSV) – Pressure pre-set with triggering by patient only.
- Synchronized Intermittent Mandatory Ventilation (SIMV) – Number of mandatory breaths (volume/pressure pre-set) is set on ventilator. Breaths are synchronized by patient triggering and patient is allowed to take spontaneous breaths in between.
- SIMV + PSV – Combination of both modes results in inspiratory support of spontaneous breath to pressure pre-set, in between mandatory breaths
Broadly there are two major modes of ventilation:
- Either volume pre-set or pressure pre-set. Other modes are derivatives of these two modes along with provision of spontaneous breathing.
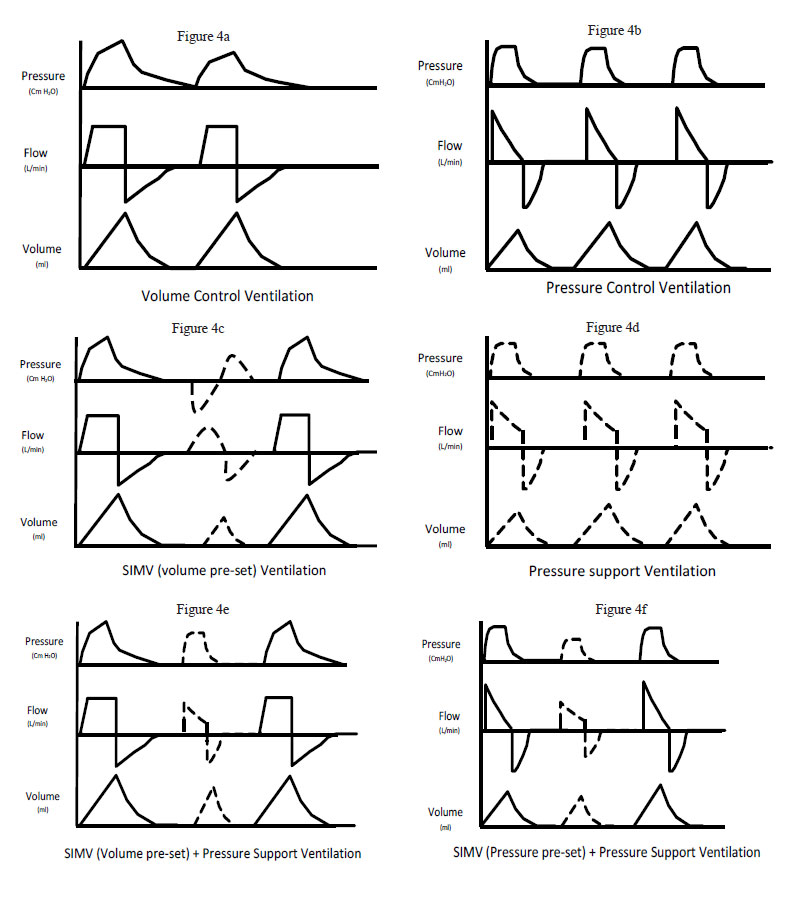
a) Assist control ventilation: AC mode is generally the initial mode of ventilation. In this, the breath is delivered either volume cycled (volume pre-set) or time cycled (pressure pre-set). A predetermined tidal volume or a predetermined applied pressure for a fixed duration is delivered at a pre-set minimal rate. The patient receives a minimum number of breaths, pre-determined on the ventilator. These breaths may be synchronized to patient’s inspiratory effort if present, and there are additional breaths to pre-set minimum rate. Therefore, the number of breaths may actually increase if there is increased number of patient’s inspiratory efforts, causing hyperventilation.
b) Synchronized intermittent mandatory ventilation: In SIMV, mandatory breaths, as pre-set on ventilator are delivered along with spontaneous breaths interspersed between mandatory breaths. These breaths again can be volume cycled or time cycled. The mandatory breaths are synchronized with patient’s spontaneous breaths, which help in better patient ventilator interaction. This mode is utilized for weaning process.
c) Pressure support ventilation: There are no mandatory breaths but all breaths are spontaneous (triggered by patient). Each spontaneous breath is augmented with positive pressure set on the ventilator. These breaths are flow cycled and help in decreasing work of breathing. This mode is utilized for weaning purpose.
Ventilator Setting
(a) Fraction of inspired oxygen (FiO2) – FiO2 is adjusted to maintain partial pressure of oxygen in arterial blood (PaO2) above 60 mmHg. If PaO2 cannot be maintained at a FiO2 of 0.5, positive end – expiratory pressure (PEEP) should be added.
(b) Minute Volume – Minute volume is a product of tidal volume and respiratory rate. It is adjusted to keep partial pressure of carbon dioxide in arterial blood (PaCO2) within acceptable limits (35–45 mmHg).
(c) Inspiratory expiratory ratio (I:E) – It is ratio of duration of inspiration to expiration. Usually this ratio is set 1:2 for normal ventilation. A ratio more than 1:1 and rapid inspiratory flow rate minimize the hemodynamic effect of positive pressure ventilation and improves oxygenation but increases PaCO2. An I:E ratio of 2:1 – 4:1 is known as inverse ratio ventilation (IRV). In IRV, the slow, long inspiration ensures distribution of ventilation to alveoli, which are slow to open up. IRV may cause dynamic hyperinflation (intrinsic PEEP) and hypercapnea.
(d) Positive end – expiratory pressure (PEEP) - This exists when airway pressure gradient is greater than ambient pressure just before the next inspiration. It is an integral part of mechanical ventilation in the management of acute alveolar pathology such as ARDS. About 4-5 cm H2O is a physiological PEEP, higher than this PEEP is indicated when it is not possible to maintain acceptable PaO2 (>60 mmHg) at FiO2 of 0.5-0.6. PEEP improves gas exchange and oxygenation at the same FiO2. PEEP also helps in recruitment of collapsed alveoli and keeps them open for ventilation, thereby minimizing the risk of shear force injury to alveoli.
Weaning of Mechanical Ventilation
Weaning is a process whereby patients are taken off from ventilator breaths to completely spontaneous breaths by decreasing the support level provided by the ventilator.
Weaning depends on the indication for which ventilatory support was initiated along with the underlying respiratory condition of the patient. As the acute condition stabilizes along with improvement in chest compliance, patient is moved down from AC mode to either SIMV or PSV with continuous assessment of patient’s condition.
Two methods are commonly used before discontinuation of mechanical ventilation, gradual reduction in pressure support and spontaneous breathing trial (SBT).
Complications associated with mechanical ventilation.
- Infection: Along with endotracheal tubes insertion, the protective reflexes of lung are blunted and this predisposes to lung infection, seen most frequently as ventilator associated pneumonia (VAP).
- Pneumothorax: The application of positive pressure to chest may cause pneumothorax if the peak inspiratory pressure reaches to a high level.
- Hypotension: If the patient is hypovolemic, conversion to positive pressure ventilation may decrease preload to heart, causing hypotension.
- Barotrauma, Volutrauma, Biotrauma: Injury to alveoli caused by increase in the peak pressure is known as barotrauma; injury caused by increased volume, volutrauma and; release of system inflammatory mediators from lungs during mechanical ventilation is known as biotrauma.
Monitoring of mechanical ventilation
Monitoring is essential to assess the beneficial and harmful effect of mechanical ventilation. This is done Pagewith the help of standard monitoring i.e. ventilator graphics, pulse oximetry, ECG, pulse, blood pressure, chest X-ray along with arterial blood gas analysis to assess the goal of ventilation.
References
- “The ICU Book” third Edition. Paul Marino
- “Text Book of Critical Care” fifth edition. Mithell P Fink et al.
- “Clinical Application of Mechanical Ventilation” third edition. David W Chang.
- Why Publish with JCPC?
- Instructions to the Authors
- Submit Manuscript
- Advertise with Us
- Journal Scientific Committee
- Editorial Policy
Print: ISSN: 2250-3528


