The Journal of Clinical and Preventive Cardiology has moved to a new website. You are currently visiting the old
website of the journal. To access the latest content, please visit www.jcpconline.org.
Review Article
Surgical Management of Morbid Obesity
Volume 1, Apr 2012
Dharmender Sharma, MBBS, MS, Anshuman Dev, MBBS, DNB, Sandeep Malhotra, MBBS, FACS, Gurgaon, India.
Volume 1, April 2012
“Let me have men around me that are fat….”
This is a quote from the first act of Shakespeare’s Julius Caesar. Perhaps at that time, higher body weight corresponded with a well-balanced mental disposition. Certainly, obesity was not a problem in those days, but now obesity has become a mammoth problem reaching epidemic proportions not only in the western countries but also in developing countries like India. It is the fastest growing chronic illness in the world today.
Magnitude of problem
In USA, approximately 5% of population or 23 million people are morbidly obese (1). Studies of adolescent obesity show that more than 35% of population in USA is obese, out of which 20% is in European population. Earlier obesity was thought to be a problem of rich and affluent people, but now it is affecting people from all strata of society. It is estimated to cause 280,000 deaths annually in USA alone, in comparison to 90,000 deaths per year from both breast and colon cancer (2). Hence, after tobacco use obesity has become the second major cause of preventable death in USA.
It is estimated that a 25-year-old morbidly obese man has 22% reduction in life expectancy. In simple terms,12 years of life are lost in comparison to a normal healthy man (2).
Closer to home, obesity has reached epidemic proportion in India too. It is estimated that 5% of Indians are morbidly obese (3). Indians are genetically susceptible to weight accumulation especially around the waist. The National Family Health Survey (NFHS) data of 2007 showed Punjab at the top of the list of obese/overweight. The percentage was 30.3% in males and 37.5% in females. The average Indian data was 12.15% and 16% for males and females, respectively (4).
Closer to home, obesity has reached epidemic proportion in India too. It is estimated that 5% of Indians are morbidly obese (3). Indians are genetically susceptible to weight accumulation especially around the waist. The National Family Health Survey (NFHS) data of 2007 showed Punjab at the top of the list of obese/overweight. The percentage was 30.3% in males and 37.5% in females. The average Indian data was 12.15% and 16% for males and females, respectively (4).
Pathophysiology and related medical problems
Pathophysiology of severe obesity is poorly understood. However, it is clear that a severely obese individual has persistent hunger that is not satiated by amounts of food that satisfy the nonobese. Basic scientific understanding of the roles played by hormones, peptides, or other factors on satiety is incomplete.
Current understanding is that some gut-related hormones play a central role in regulating weight in individuals. Ghrelin is produced and released from enteroendocrine X/A-like cells (5) in the gastric fundus mucosa. Peripheral administration of ghrelin causes weight gain by reducing fat utilization and stimulating food intake in rats (6). Ghrelin also suppresses insulin in humans (7). Serum ghrelin concentrations are increased by fasting and reduced by refeeding in rats and humans (8). GIP is synthesized and released by K-cells of the duodenum and proximal jejunum in response to glucose and fat ingestion. In type 2 diabetes, GIP is attenuated secondary to decreased expression of GIP receptors (9). GLP-1 and PYY are produced and secreted from endocrine L-cells in the mucosa of the ileum and colon. GLP-1 is a major contributor to the ileal brake mechanism of the upper GI tract by slowing gastric emptying of both liquids and solids (10,11). That is why the metabolic requirements for insulin after food intake are reduced or at least delayed (12). Intravenous administration of GLP-1 reduces food intake with ratings of reduced hunger and increased fullness (13–15). It also reduces the rate of gastric emptying. The truncated form of PYY is released from the GI tract after a meal and induces satiety (16). Postprandial plasma PYY concentrations have recently been shown to be lower in obese than lean subjects (17). PYY also inhibits fasting small bowel motility (18) and gastric emptying (19).
Obesity affects every system of the body. It increases the risk of illness from around 30 serious medical conditions. The most frequent problem faced by an obese individual is arthritis and degenerative joint disease effecting at least 50% of individual seeking surgery. However, incidence of gastroesophageal reflux (GERD) is in 20–30% patients, hypertension in 30%, NIDDM in 20%, and asthma in 25% (20). Numerous other health problems that may occur with obesity include cardiovascular disease, depression, dyslipidemia, infertility, metabolic syndrome, mortality, nonalcoholic fatty liver disease, obstructive sleep apnea, urinary stress incontinence, and venous stasis disease. These are excluding the everyday problems like usage of toilets, seating, use of public transportation, workplace discrimination, and low selfesteem.
Medical versus surgical therapy
Although this article mainly focuses on the surgical treatment of obesity, it is well known that medical therapy has limited short-term and almost nonexistent long-term success. The likelihood that a severely obese person will lose weight by dietary means alone and remain at BMI below 35 kg/m2 is 3% or less (20).
Current understanding is that some gut-related hormones play a central role in regulating weight in individuals. Ghrelin is produced and released from enteroendocrine X/A-like cells (5) in the gastric fundus mucosa. Peripheral administration of ghrelin causes weight gain by reducing fat utilization and stimulating food intake in rats (6). Ghrelin also suppresses insulin in humans (7). Serum ghrelin concentrations are increased by fasting and reduced by refeeding in rats and humans (8). GIP is synthesized and released by K-cells of the duodenum and proximal jejunum in response to glucose and fat ingestion. In type 2 diabetes, GIP is attenuated secondary to decreased expression of GIP receptors (9). GLP-1 and PYY are produced and secreted from endocrine L-cells in the mucosa of the ileum and colon. GLP-1 is a major contributor to the ileal brake mechanism of the upper GI tract by slowing gastric emptying of both liquids and solids (10,11). That is why the metabolic requirements for insulin after food intake are reduced or at least delayed (12). Intravenous administration of GLP-1 reduces food intake with ratings of reduced hunger and increased fullness (13–15). It also reduces the rate of gastric emptying. The truncated form of PYY is released from the GI tract after a meal and induces satiety (16). Postprandial plasma PYY concentrations have recently been shown to be lower in obese than lean subjects (17). PYY also inhibits fasting small bowel motility (18) and gastric emptying (19).
Obesity affects every system of the body. It increases the risk of illness from around 30 serious medical conditions. The most frequent problem faced by an obese individual is arthritis and degenerative joint disease effecting at least 50% of individual seeking surgery. However, incidence of gastroesophageal reflux (GERD) is in 20–30% patients, hypertension in 30%, NIDDM in 20%, and asthma in 25% (20). Numerous other health problems that may occur with obesity include cardiovascular disease, depression, dyslipidemia, infertility, metabolic syndrome, mortality, nonalcoholic fatty liver disease, obstructive sleep apnea, urinary stress incontinence, and venous stasis disease. These are excluding the everyday problems like usage of toilets, seating, use of public transportation, workplace discrimination, and low selfesteem.
Medical versus surgical therapy
Although this article mainly focuses on the surgical treatment of obesity, it is well known that medical therapy has limited short-term and almost nonexistent long-term success. The likelihood that a severely obese person will lose weight by dietary means alone and remain at BMI below 35 kg/m2 is 3% or less (20).
Eligibility for Bariatric surgery
Preoperative selection for bariatric surgery for patients in western countries is based on National Institute of Health consensus guidelines, which says that patients with BMI >40 kg/m2 without any comorbid medical conditions or 35 kg/m2 with associated comorbid problems (21). Patients should also have failed dietary therapy. They should also be mentally stable, motivated, and knowledgeable about the surgery and its complication. And of course patient should be medically fit for surgery.
The criteria are different for Asian patients as they are prone to obesity-related illnesses at a lower BMI. So an Asian patient with BMI >37.5 kg/m2 without any comorbid medical conditions or 32.5 kg/m2 with associated comorbid problems is to be considered for bariatric surgery (22).
The criteria are different for Asian patients as they are prone to obesity-related illnesses at a lower BMI. So an Asian patient with BMI >37.5 kg/m2 without any comorbid medical conditions or 32.5 kg/m2 with associated comorbid problems is to be considered for bariatric surgery (22).
Surgical options
Bariatric surgery can broadly be divided into three categories:
- Restrictive procedures
Laparoscopic adjustable gastric banding
- Largely restrictive/mildly malabsorbtive procedures
Laparoscopic Roux- en- Y gastric bypass
- Largely malabsorbtive/mildly restrictive procedures
Biliopancreatic diversion
Biliopancreatic diversion with duodenal switch
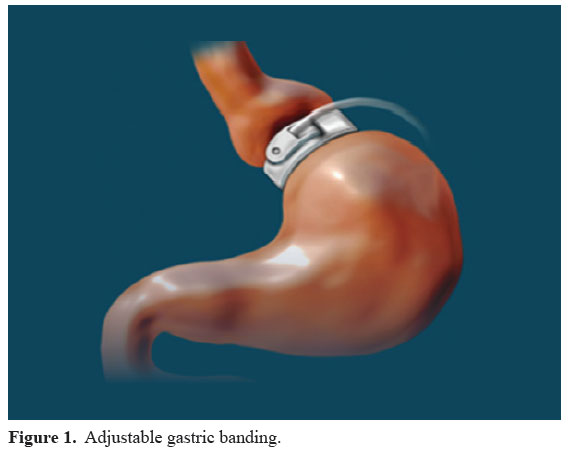
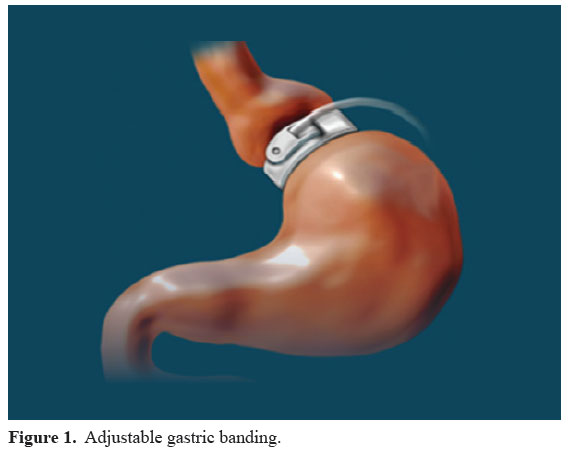
Laparoscopic adjustable gastric banding (LAGB)
In this procedure, an inflatable silicon band is placed in the upper part of stomach which restricts the oral intake by limiting the volume of proximal stomach. This band is connected through a tubing to the infusion port placed in a subcutaneous pocket on the abdominal wall (Fig. 1) This is a simple and reversible procedure for obesity. Initially the band is not distended; consequently saline is added in 1–1.5 mL increments to produce a desired weight loss of 1–2 kg per week. Plateau of weight and increased hunger are usually indications to fill the band further.
The advantage of this procedure is low incidence of metabolic problems, no disturbance of normal GI tract, simplicity, safety, and reversibility.
Disadvantage is potential for slippage, dilatation of esophagus, and erosion into stomach.
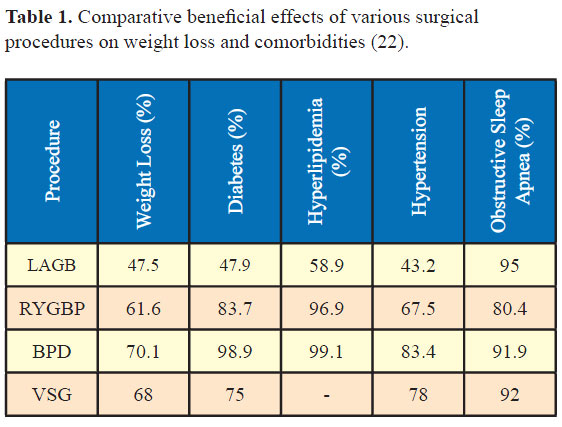
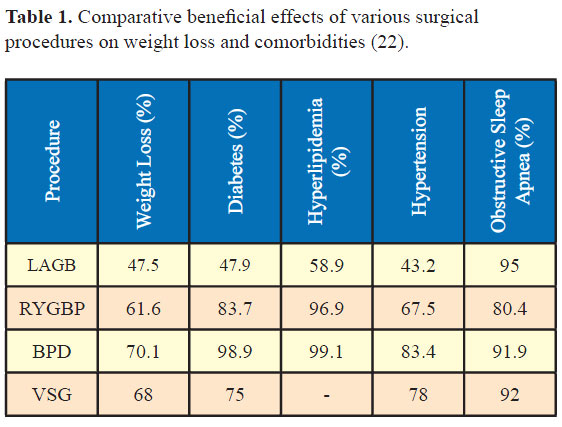
Average weight loss is between 40% and 50% at 2 years and maximum weight loss is generally achieved by third year of surgery. Diabetes remission is achieved in 48% patients and improvement in 70–80%. Dyslipidemia improves in 60% of patients (23).
This surgery takes around 30–40 minutes of operative time and needs hospitalization for a day.
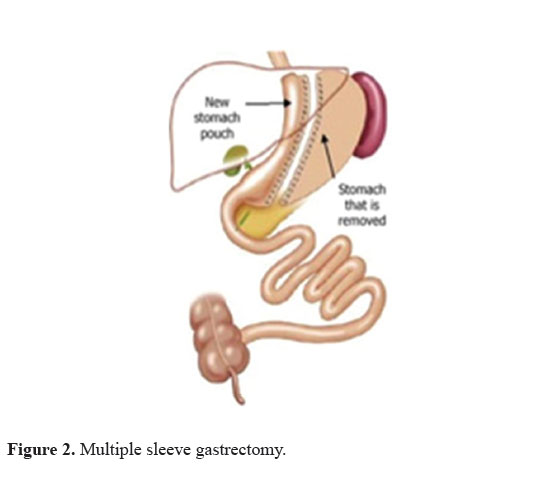
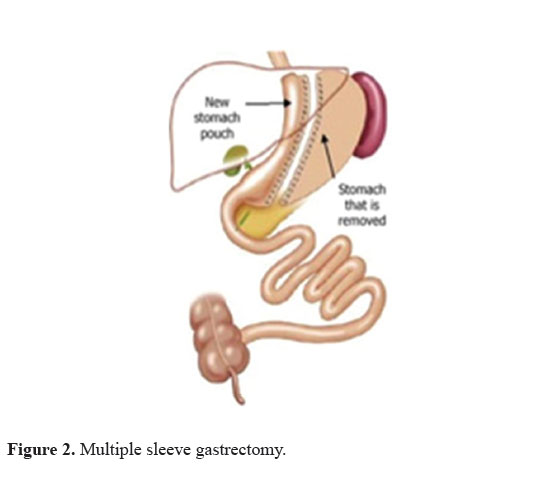
Laparoscopic vertical sleeve gastrectomy (VSG)
In this procedure, approximately two-third of the stomach is removed using surgical staplers which cut and join the stomach walls simultaneously, leaving a banana shaped stomach with a capacity of 100–150 mL (Fig. 2).
Advantage is that it does not alter the physiology of GI tract to any major degree, technically a simpler operation, and there is no fear of malabsorption. Patients achieve loss of 60–70% weight at 2 years time, 90–98% resolution of diabetes, hypertension, dyslipidemia, sleep apnea, and arthritis.
Disadvantage is that it is a technically more advanced surgery and risk of staple line leak is always present.
Operative time is around 90 minutes and patient needs to stay for a day at hospital. Before discharge, a dye study is done to rule out any leak through the anastomosis site.
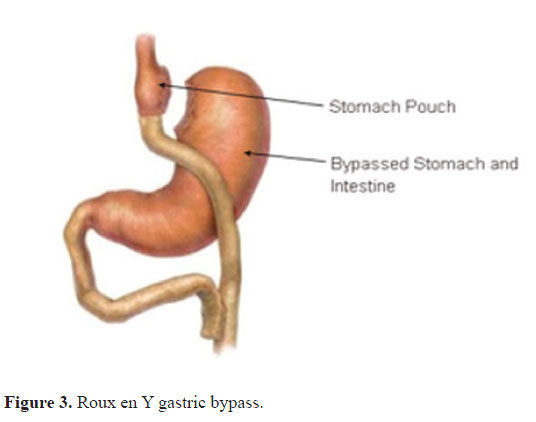
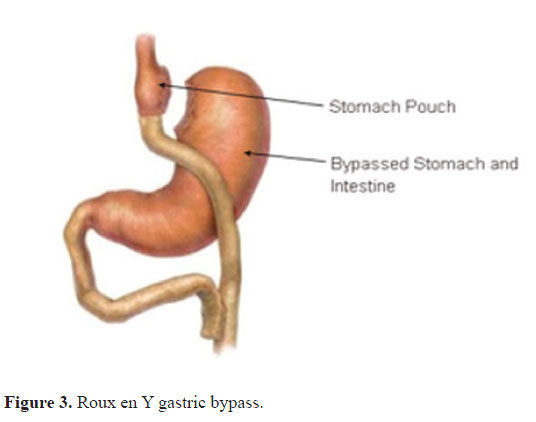
Roux en Y-gastric bypass (RYGB)
This procedure is considered the gold standard of all the bariatric procedures.
In this procedure, surgical staplers are used to create a small pouch of around 10–15 mL capacity in upper part of stomach and the larger part of stomach and intestine is bypassed (Fig. 3). Thus that food and digestive juices come in contact with each other in the later part in the GI system. This leads to delay and reduction in absorption of nutrients and calories.
The advantage is a higher weight loss averaging 60–70%. It is also reported to have a faster and more durable weight loss.
The disadvantage is a slightly higher risk of early postoperative complications and mortality. Also the patient needs to be compliant enough to take lifelong supplementation of vitamins and micronutrients. This is definitely a big problem in Indian scenario, given the general noncompliance, once the goal of weight loss is achieved.
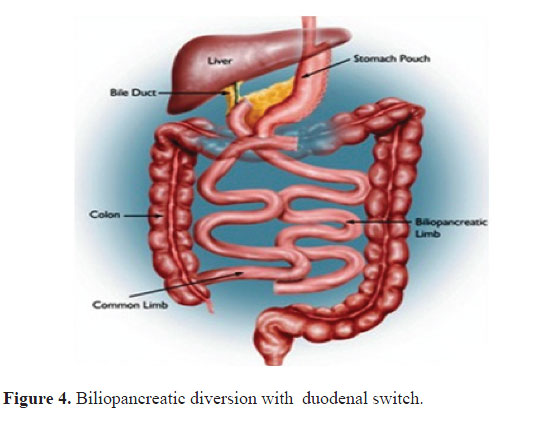
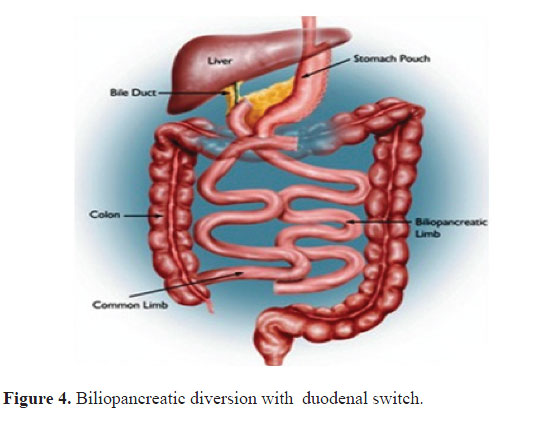
Biliopancreatic diversion with duodenal switch (BPDDS)
This procedure is based on a smaller stomach and combines a lower restriction and a high level of malabsorption. In this procedure, approximately twothird of stomach is removed and intestines are rearranged so that the area where the food mixes with digestive uices is short (Fig. 4).
This procedure is claimed to cause the maximal weight loss of around 70% (24) at 2 years and resolution of diabetes (98%) but has the highest mortality rates among all procedures (0.9–1.1%) and a higher risk of vitamin and protein malnutrition (24,25).
This procedure is claimed to cause the maximal weight loss of around 70% (24) at 2 years and resolution of diabetes (98%) but has the highest mortality rates among all procedures (0.9–1.1%) and a higher risk of vitamin and protein malnutrition (24,25).
It is generally advised for the super super obese, having a BMI of >60 kg/m2.
Resolution of comorbidities after bariatric surgery
For those having undergone bariatric surgery, about 95% of patients are able to maintain long-term weight loss (25). Nine-six percent of patients experienced quality of life improvement (26) and 89% saw a reduction in the relative risk of mortality over a 5-year period (27). In a clinical study, gastric bypass surgery reduced the total number of comorbidities of participating patients by 96%. Depression improved in 47% of patients, and osteoarthritis and joint pain resolved in 41% of patients (28).
Complications after bariatric surgery
BBariatric surgery is safe for the patients and complications are few if prophylactic measures are taken and postoperative follow-up is good. Complications of bariatric surgery can be separated into complications associated with surgery, complications due to obesity, and side-effects associated with the alterations in the upper GI tract anatomy. The perioperative mortality of bariatric surgery is less than 1% and is usually associated with anastamotic leaks with peritonitis (75%) or pulmonary embolism (25%). Most common complications are related to the patient’s obesity and include DVT, PE, pulmonary atelectasis or pneumonia, and myocardial infarction. These are easily prevented by thorough preoperative cardiac and pulmonary testing, and prophylactic measures like early ambulation, DVT prophylaxis, and spirometry.
LAGB can be complicated by band slippage, erosion into stomach, esophageal dilatation, and tubing or port complications like infection of port, tubing disconnection, and saline leak from the band. Nutrient deficiency is rare and multivitamin supplements are recommended but not critical.
Early complications of RYGB surgery include anstamosis leak or bleeding, stenosis at gastrojejunostomy, marginal ulcers, dumping syndrome and acute gastric distention secondary to edema, and obstruction at entero-enterostomy. Long-term complications include internal hernias, and deficiency of iron, calcium, vitamin B12, protein, or micronutrients. The nutrient deficiency can be prevented with proper supplements and diligent follow-up.
VSG can be complicated by bleeding, staple line leak, stenosis of sleeve, or esophageal reflux. Nutrient deficiency can occur but is rare as there is no malabsorption and supplements are recommended bur not critical.
Conclusion
Bariatric surgical procedures are an effective method to control morbid obesity and its associated comorbidities. But, each procedure has its own unique advantages and limitations and should be carefully chosen, properly performed, and diligently followed. It should also be kept in mind that these are not cosmetic procedures and should be used only when medically indicated and lifestyle modification efforts have failed.
In the Indian scenario, restrictive procedures like LAGB and VSG are more suitable as long-term vitamin supplements are not critical and patients are likely to be safe even if they are noncompliant with supplements and follow-up. VSG seems to be the ideal bariatric operation for the Indian patient as the weight loss and improvement in diabetes appear to be better than with laparoscopic adjustable gastric banding and on par with Roux-en-Y gastric bypass (29).
Funding sources
None
Disclosures
None
References
References
- Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity amongst UD adults.1999-2000.JAMA.2002; 288:1723-7.
- Fontaine KR, Redden DT, Wang C, Westfall AO, Allison DB. Years of life lost due to obesity. JAMA. 2003; 289:187-93.
- India facing obesity epidemic. Experts, The Hindu, 2007,10-12
- 3rd National Family Health Survey, Mumbai:International institute for population sciences, 2006.
- Date Y, Kojima M, Hosoda H, Sawaguchi A, Mondal MS, Suganuma T, Matsukura S, Kangawa K, Nakazato M. Ghrelin, a novel growth hormone-releasing acylated peptide, is synthesized in a distinct endocrine cell type in the gastrointestinal tracts of rats and humans. Endocrinology. 2000; 141(11):4255-61.
- Tschöp M, Smiley DL, Heiman ML. Ghrelin induces adiposity in rodents. Nature. 2000 19; 407(6806):908-13.
- Broglio F, Arvat E, Benso A, Gottero C, Muccioli G, Papotti M, van der Lely AJ, Deghenghi R, Ghigo E. Ghrelin, a natural GH secretagogue produced by the stomach, induces hyperglycemia and reduces insulin secretion in humans. J Clin Endocrinol Metab. 2001; 86(10):5083-6.
- Tschöp M, Wawarta R, Riepl RL, Friedrich S, Bidlingmaier M, Landgraf R, Folwaczny C. Post-prandial decrease of circulating human ghrelin levels. J Endocrinol Invest. 2001; 24(6):RC19-21.
- Miyawaki K, Yamada Y, Yano H, Niwa H, Ban N, Ihara Y, Kubota A, Fujimoto S, Kajikawa M, Kuroe A, Tsuda K, Hashimoto H, Yamashita T, Jomori T, Tashiro F, Miyazaki J, Seino Y. Glucose intolerance caused by a defect in the entero-insular axis: a study in gastric inhibitory polypeptide receptor knockout mice. Proc Natl Acad Sci U S A. 1999; 96(26):14843-7.
- Näslund E, Bogefors J, Skogar S, Grybäck P, Jacobsson H, Holst JJ, Hellström PM. GLP-1 slows solid gastric emptying and inhibits insulin, glucagon, and PYY release in humans. Am J Physiol. 1999; 277(3 Pt 2):R910-6.
- Wettergren A, Schjoldager B, Mortensen PE, Myhre J, Christiansen J, Holst JJ. Truncated GLP-1 (proglucagon 78-107-amide) inhibits gastric and pancreatic functions in man. Dig Dis Sci. 1993; 38(4):665-73.
- Nauck MA, Niedereichholz U, Ettler R, Holst JJ, Orskov C, Ritzel R, Schmiegel WH. Glucagon-like peptide 1 inhibition of gastric emptying outweighs its insulinotropic effects in healthy humans. Am J Physiol. 1997; 273(5 Pt 1):E981-8.
- Flint A, Raben A, Astrup A, Holst JJ. Glucagon-like peptide 1 promotes satiety and suppresses energy intake in humans. J Clin Invest. 1998; 101(3):515-20.
- Näslund E, Barkeling B, King N, Gutniak M, Blundell JE, Holst JJ, Rössner S, Hellström PM. Energy intake and appetite are suppressed by glucagon-like peptide-1 (GLP-1) in obese men. Int J Obes Relat Metab Disord. 1999 Mar;23(3):304-11.
- Verdich C, Flint A, Gutzwiller JP, Näslund E, Beglinger C, Hellström PM, Long SJ, Morgan LM, Holst JJ, Astrup A. A meta-analysis of the effect of glucagon-like peptide-1 (7-36) amide on ad libitum energy intake in humans. J Clin Endocrinol Metab. 2001; 86(9):4382-9.
- Batterham RL, Cowley MA, Small CJ, Herzog H, Cohen MA, Dakin CL, Wren AM, Brynes AE, Low MJ, Ghatei MA, Cone RD, Bloom SR. Gut hormone PYY(3-36) physiologically inhibits food intake. Nature. 2002; 418(6898):650-4.
- Batterham RL, Cohen MA, Ellis SM, Le Roux CW, Withers DJ, Frost GS, Ghatei MA, Bloom SR. Inhibition of food intake in obese subjects by peptide YY3-36. N Engl J Med. 2003; 349(10):941-8.
- Al-Saffar A, Hellström PM, Nylander G. Correlation between peptide YY-induced myoelectric activity and transit of small-intestinal contents in rats. Scand J Gastroenterol. 1985; 20(5):577-82.
- Savage AP, Adrian TE, Carolan G, Chatterjee VK, Bloom SR. Effects of peptide YY (PYY) on mouth to caecum intestinal transit time and on the rate of gastric emptying in healthy volunteers. Gut. 1987; 28(2):166-70.
- William OR, Bruce DS. Morbid obesity. Chapter 17, Sabiston textbook of Surgery, 18ed
- Gastrointestinal surgery for severe obesity: National Institutes of Health Consensus Development Conference Statement. Am J Clin Nutr. 1992; 55(2 Suppl):615S-619S.
- Misra A, Chowbey P, Makkar BM, Vikram NK, Wasir JS, Chadha D, Joshi SR, Sadikot S, Gupta R, Gulati S, Munjal YP; Concensus Group. Consensus statement for diagnosis of obesity, abdominal obesity and the metabolic syndrome for Asian Indians and recommendations for physical activity, medical and surgical management. J Assoc Physicians India. 2009; 57:163-70.
- Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, Schoelles K. Bariatric surgery: a systematic review and metaanalysis. JAMA. 2004; 292(14):1724-37.
- Maggard MA, Shugarman LR, Suttorp M, Maglione M, Sugerman HJ, Livingston EH, Nguyen NT, Li Z, Mojica WA, Hilton L, Rhodes S, Morton SC, Shekelle PG. Meta-analysis: surgical treatment of obesity. Ann Intern Med. 2005 5;142(7):547-59.
- http://www.bariatric.us/bariatric-surgery-results.html
- Schauer PR, Ikramuddin S, Gourash W, Ramanathan R, Luketich J. Outcomes after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Ann Surg. 2000; 232(4):515-29.
- Christou NV, Sampalis JS, Liberman M, Look D, Auger S, McLean AP, MacLean LD. Surgery decreases long-term mortality, morbidity, and health care use in morbidly obese patients. Ann Surg. 2004; 240(3):416-23; discussion 423-4.
- http://www.realize.com/gastric-bypass-surgery-benefits.htm
- Deitel M, Gagner M, Erickson AL, Crosby RD. Third International Summit: Current status of sleeve gastrectomy. Surg Obes Relat Dis. 2011; 7(6):749-59.
- Why Publish with JCPC?
- Instructions to the Authors
- Submit Manuscript
- Advertise with Us
- Journal Scientific Committee
- Editorial Policy
Print: ISSN: 2250-3528


