The Journal of Clinical and Preventive Cardiology has moved to a new website. You are currently visiting the old
website of the journal. To access the latest content, please visit www.jcpconline.org.
Brief Report
Role of Folate in Management of Endothelial Dysfunction
Volume 2, Apr 2013
Upinder Kaur, MBBS, B.L. Pandey, MD, PhD (Medicine), PhD (Ayu), Varanasi,UP, India
J Clin Prev Cardiol 2013;2(2):91-4
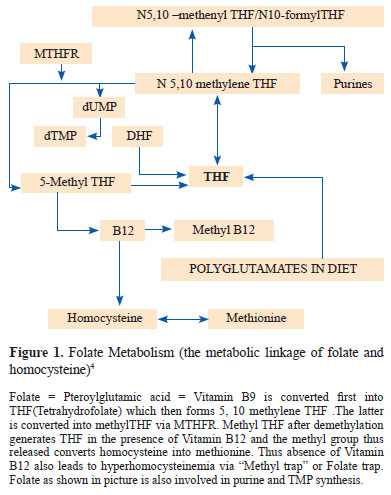
IntroductionEndothelial dysfunction is considered as a hallmark in the pathogenesis of many cardiovascular disorders like myocardial infarction (MI), angina, stroke and diabetes (1, 2). It is a long-term predictor of the development of atherosclerosis and cardiovascular events and a useful surrogate marker for cardiovascular disease. A number of factors have been attributed to this including hyperlipidemia, hypertension, smoking, obesity and hyperhomocysteinemia (3). Elevated homocysteine levels affect endothelium by a number of ways such as generating excess of reactive oxygen species, causing peroxidation of lipids, impairing nitric oxide (NO) and direct endothelial toxicity (4). Homocysteine damages endothelium and decreases its ability to produce NO in response to stress and pharmacological stimuli by modifying eNOS activity (5). Further intracellular superoxides O2 and peroxynitrites ONOO- have been found to increase with elevated homocysteine levels. Folate supplementation has been associated with reduced cardiovascular risk by decreasing homocysteine levels. Further, high single-dose and multiple-dose folic acid administration has been shown to prevent the temporary endothelial dysfunction induced by post-methionine-load hyperhomocysteinemia (6). But recent studies show a vasculoprotective action of folate independent of homocysteine diminution (7).
Proposed Mechanisms of Folate in Cardiovascular Protection
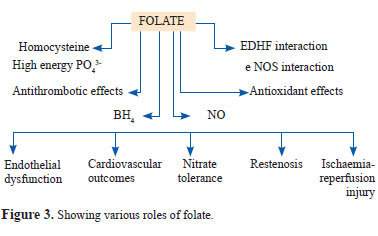
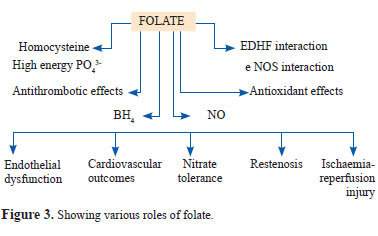
A number of actions of folate are considered responsible for its endothelial protective role.
Reduction of Hyperhomocysteinemia
Since homocysteine is a definite contributor to cardiovascular risk (8), homocysteine conversion to methionine is supposed to be a key beneficial consequence of folate administration. Folate administration augments endothelial function assessed by ultrasound guided flow mediated dilation of brachial artery (9). Studies have shown significant reduction in homocysteine profiles in asymptomatic patients with hyperhomocysteinemia as well as in patients with coronary artery disease with elevated homocysteine which suggests homocysteine lowering by folate as an important mechanism (10,11). On the other hand in patients of homocysteinuria (serum homocysteine >300 μmol/L), with very high risk of developing coronary event, folate treatment led to remarkable reduction in oxidative stress and improvement in endothelial dysfunction without proportional reduction in levels of homocysteine (12). MTHF (Methyl tetrahydrofolate) supplementation has also improved endothelial function in hypercholesterolemic patients without elevated levels of homocysteine (13). Even in those with significant coronary artery disease, endothelial protective action of folate was demonstrated independent of lowering of homocysteine levels (7). Vasculoprotective action of folate was found in one study to correlate better with reduction in free but not total homocysteine (14).
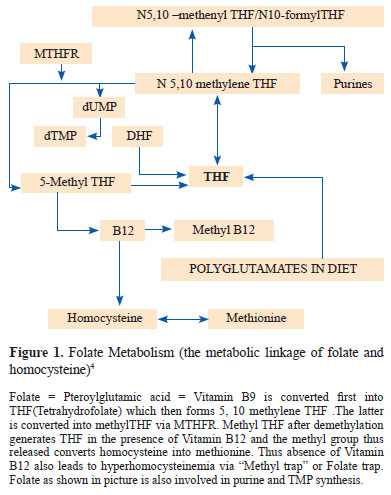
It has been recently demonstrated that 5-methyl tetrahydrofolate 5 MTHF is the key regulator of eNOS coupling and NO availability in vessels and that homocysteine serves as an indirect regulator. Further folate supplementation in diabetic patients has been shown to improve insulin resistance (20). The endothelial protective effects of folate are seen at high doses and in early stages of atherogenesis (21). Only modest benefit is seen in the presence of advanced coronary artery disease and none in patients with end stage renal failure (22). Studies like Kuopio Ischaemic Heart Disease isk Factor Study, the Framingham Heart Study, National health and Nutrition Examination Survey have displayed an inverse relationship between serum folate and cardiovascular risk, although not supported by some groups (23). Nutrients, predominantly the vitamins, phytochemicals, types of fats and physical activity profiles have diverse molecular implications for the prevention and management of chronic inflammatory conditions (24).
Antioxidant action
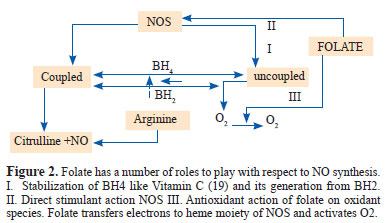
Oxidative stress results from disequilibrium between the production of reactive oxygen species (ROS) and the tissue antioxidant defenses. Excess ROS formation is observed in conditions like diabetes, myocardial infarction, angina, congestive heart failure and Alzheimer’s dementia (15). Reactive oxygen species interact with NO and form toxic peroxynitrite radicals with detrimental effects like oxidation of BH4 (tetrahydrobiopterin), degradation of zinc-thiolate cluster involved in eNOS (nitric oxide synthase) coupling and degradation of GTP Cyclohydrolase (GTPCH1) enzyme involved in BH4 synthesis. All these culminate in eNOS uncoupling so that NOS becomes a net producer of O2 - and NO level in endothelium falls (16). Endothelial dysfunction is hence consequent to reduced bioavailability of endothelium-derived NO. MTHF has been shown to reduce the generation of oxidant species via its interaction with hypoxanthine/xanthine oxidase and eNOS (13). Folate deficiency in rats has been linked to high lipid peroxidati n and reduced antioxidant defense mechanisms (17).
Interactions with eNOS
A pteridine binding site for folate has been demonstrated on eNOS as is on DHFR (dihydrofolatereductase) (18). eNOS enzyme is involved in NO synthesis in endothelium which is responsible for vasodilation in response to stress or pharmacological stimuli. It binds NADPH at the N terminal oxygenase site and O2, BH4 and arginine at the C terminal reductase site. BH4 (tetrahydrobiopterin) is required for coupling of eNOS to NO synthesis. Folate has been shown to potentiate NO action and synthesis as depicted in Figure 2.
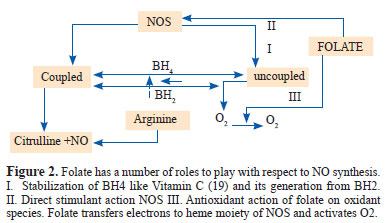
It has been recently demonstrated that 5-methyl tetrahydrofolate 5 MTHF is the key regulator of eNOS coupling and NO availability in vessels and that homocysteine serves as an indirect regulator. Further folate supplementation in diabetic patients has been shown to improve insulin resistance (20). The endothelial protective effects of folate are seen at high doses and in early stages of atherogenesis (21). Only modest benefit is seen in the presence of advanced coronary artery disease and none in patients with end stage renal failure (22). Studies like Kuopio Ischaemic Heart Disease isk Factor Study, the Framingham Heart Study, National health and Nutrition Examination Survey have displayed an inverse relationship between serum folate and cardiovascular risk, although not supported by some groups (23). Nutrients, predominantly the vitamins, phytochemicals, types of fats and physical activity profiles have diverse molecular implications for the prevention and management of chronic inflammatory conditions (24).
Folic acid –B12 supplementation study in obese Type 2 diabetes patients (25)
A trial of assessing improvement in endothelial function by flow mediated dilatation of brachial artery after supplementation of folate at 5 mg and vitamin B12 at 500 μg in 32 obese patients with type 2 diabetes and BMI >25 kg/m2 revealed uniform and highly significant improvement in endothelial function in folate group. No significant improvement was noticed in the control group (25).
Folate sufficiency was initially considered to be merely the absence of anemia. Reminiscence in folate biology has occurred since the demonstration of neural tube defects in infants born to folate deficient mothers. Now it is well supported that folate deficiency is associated with increased cardiovascular risk. Amount present in diet is not sufficient to prevent the risk of cardiovascular disease particularly when diet includes animal products which increase methionine in serum. The inconsistencies project strong imperatives for adequate translational efforts to define and diagnose appropriate indications, personalized contexts, optimal dose and synergetic nutrient regimens toward exploiting great promise of the simple and most economical vitamin. The critical methyl-donor role of folate singularly emphasizes its therapeutic significance for almost all the chronic diseases of modern times which take root in phenotypes caused by epigenetic distortions. The significant benefit of folate–B12 supplement in obese diabetics reaped uniformly and rapidly in our referred study further endorses this and calls for renewed explorations to attain personalized medicine of folate in meeting the challenge of coronary artery disease.
References
Conclusion
Folate sufficiency was initially considered to be merely the absence of anemia. Reminiscence in folate biology has occurred since the demonstration of neural tube defects in infants born to folate deficient mothers. Now it is well supported that folate deficiency is associated with increased cardiovascular risk. Amount present in diet is not sufficient to prevent the risk of cardiovascular disease particularly when diet includes animal products which increase methionine in serum. The inconsistencies project strong imperatives for adequate translational efforts to define and diagnose appropriate indications, personalized contexts, optimal dose and synergetic nutrient regimens toward exploiting great promise of the simple and most economical vitamin. The critical methyl-donor role of folate singularly emphasizes its therapeutic significance for almost all the chronic diseases of modern times which take root in phenotypes caused by epigenetic distortions. The significant benefit of folate–B12 supplement in obese diabetics reaped uniformly and rapidly in our referred study further endorses this and calls for renewed explorations to attain personalized medicine of folate in meeting the challenge of coronary artery disease.
References
- Schalkwijk CG, Stchouver CD. Vascular complications in Diabetes mellitus: The role of endothelial dysfunction. Clin Sci. 2005;109:143-59.
- Schachinger V, Britten MB, Zeiher AM. Prognostic impact of coronary vasodilator dysfunction on adverse long term outcome of coronary heart disease. Circulation. 2000;101:1899-906.
- Hadi HA, Carr CS, Suwaidi JA. Endothelial Dysfunction: Cardiovascular Risk Factors, Therapy and outcome. Vasc Health Risk Manag. 2005;1:183-98.
- Stanger O, Wonisch W. Enzymatic and non-enzymatic anti-oxidative effects of Folic acid and its reduced derivatives. Subcell Biochem. 2012;56:131-61.
- He L, Zeng H, Li F, Feng J, Liu S, Liu J, Yu J, Mao J, Hong T, Chen AF, Wang X, Wang G. Homocysteine impairs coronary artery endothelial function by inhibiting tetrahydrobiopterin in patients with hyperhomocysteinemia. Am J Physiol Endocrinol Metab. 2010;299:E1061-5.
- Chao CL, Chien KL, Lee YT. Effect of short term Vitamin (Folic acid, Vitamin B6 and Vitamin B12) administration on endothelial dysfunction induced by post Methionine load hyperhomocysteinemia. Am J Cardiol. 1999;84:1359-61.
- Doshi SN, McDowell IFW, Moat SJ, Payne N, Durrant HJ, Lewis MJ, Goodfellow J. Folic acid improves endothelial function in coronary artery disease via mechanisms largely independent of Homocysteine lowering. Circulation. 2002;105:22-6.
- Wald DS, Law M, Morris JK. Homocysteine and cardiovascular disease: evidence on causality from a meta-analysis. BMJ 2002;325:1202.
- Corretti MC, Anderson TJ, Benjamin EJ, Celermajer D, Charbonneau F, Creager MA, Deanfield J, Drexler H, Gerhard – Herman M, Herrington D, Vallance P, Vita J, Vogel R. Guidelines for the ultrasound assessment of endothelial – dependent flow mediated vasodilation of brachial artery: A report of the International Brachial Artery Reactivity Task Force. J Am Coll Cardiol .2002;39:257-65.
- Woo KS, Choo KP, Lolin YI, Sanderson JE, Metriweli C, Celermajer DS. Folic acid improves arterial endothelial function in adults with hyperhomocysteinemia. J Am Coll Cardiol. 1999;33:2002-6.
- Bellamy MF, McDowell IFW, Ramsey MW, Brownlee M, Newcombe RG, Lewis MJ. Oral Folate enhances endothelial function in hyperhomocysteinemia subjects. Eur J Clin Invest. 1999;29:659-62.
- Sugamura K, Keaney JF Jr. Reactive Oxygen Species in Cardiovascular Disease. Free Radic Biol Med. 2011;51:978-92.
- Verhaar MC, Wever RM, Kastelein JJ, van Dam T, Koomans HA, Rabelink TJ. 5-Methyl tetrahydrofolate, the active form of folic acid, restores endothelial function in familial hypercholesterolemia. Circulation. 1998;97:237-241.
- Chambers JC, Ueland PM, Obeid AO, Wrigley J, Refsum H, Kooner SJ. Improved vascular function after oral B vitamins: an effect mediated through reduced concentrations of free plasma homocysteine. Circulation. 2000;102:2479-83.
- Yap S, Naughten ER, Wilcken B, Wilcken DE, Boers GH. Vascular complications of severe hyperhomocysteinemia in patients with homocystinuria due to cystathionine beta-synthase deficiency: effects of homocysteine-lowering therapy. Semin Thromb Hemost. 2000;26:335–40
- Verhaar MC, Stroes E, Rabelink TJ. Folates and cardiovascular disease. Arterioscler Thromb Vasc Biol. 2002;22: 6-13.
- Durrand P, Prost M, Blache D. Prothrombotic effects of a Folic acid deficient diet in rat platelets and macrophages related to elevated homocysteine and decreased n-3 polyunsaturated fatty acids. Atherosclerosis. 1996;121:231-43.
- Mayer B, Pitters E, Pfeiffer S, Kukovetz WR, Schmidt K. A synthetic peptide corresponding to putative Dihydrofolatereductase domain of Nitric oxide synthase inhibits uncoupled NADPH oxidation. Nitric Oxide 1997;1:50-5.
- Heller R, Unbehaun A, Schellenberg B, Mayer B, Werner-Felmayer G, Werner ER. L-Ascorbic acid potentiates endothelial Nitric oxide synthesis via a chemical stabilization of Tetrahydrobiopterin. J Biol Chem. 2001;276:40-7.
- Setola E, Monti LD, Galluccio E, Palloshi A, Fragasso G, Paroni R, Magni F, Sandoli EP, Lucotti P, Costa S, Fermo I, Galli- Kienle M, Origgi A, Margonato A, Piatti P. Insulin resistance and endothelial function are improved after folate and vitamin B12 therapy in patients with metabolic syndrome: Relationship between Homocysteine levels and hyperinsulinemia. Eur J Endocrinol. 2004;151:483-9.
- Moat SJ, Madhavan A, Taylor SY, Payne N, Allen RH, Stabler SP, Goodfellow J, McDowell IF, Lewis MJ, Lang D. High but not low dose folic acid improves endothelial function in coronary artery disease. Eur J Clin Invest. 2006;36:850-9.
- van Guldener C, Janssen MJ, Lambert J, ter Wee PM, Jakobs C, Donker AJM, Stehouwer CDA. No change in impaired endothelial function after long term folic acid therapy of hyperhomocysteinemia in hemodialysis patients. Nephro Dial Transplant. 1998;13:106-12.
- Voutilainen S, Rissanen TH, Virtanen J, Lakka TA, Salonen JT. Low dietary folate intake is associated with an excess incidence of acute coronary events: the Kuopio Ischemic Heart Disease Risk Factor Study. Circulation. 2001;103:2674-80.
- Pandey G, Pandey AK. Nutrition research perspectives in autoinflammatory disorders. Indian J Rheumatol. 2013;(In press).
- Kaur U, Agrawal NK, Shukla RC, Pandey BL. Uniform improvement in endothelial function following Folate- Vitamin B12 supplementation in obese Type 2 Diabetes Mellitus patients. Quart JSurg Sci. 2012;1:17-22.
- Why Publish with JCPC?
- Instructions to the Authors
- Submit Manuscript
- Advertise with Us
- Journal Scientific Committee
- Editorial Policy
Print: ISSN: 2250-3528


