The Journal of Clinical and Preventive Cardiology has moved to a new website. You are currently visiting the old
website of the journal. To access the latest content, please visit www.jcpconline.org.
Debate - Part 1
Prosthetic Valve Obstruction – Thrombolysis Is a Good Option in Majority of Patients
Volume 1, Oct 2012
Sanjeev Gera DNB, Ashok K. Omar, MD, Sameer Shrivastava, MD, DM, New Delhi, India
J Clin Prev Cardiol 2012;1(4):185-9
Prosthetic valve obstruction is rare but a life-threatening complication after cardiac valve replacement associated with significant morbidity and mortality warranting immediate management. Incidence of prosthetic valve thrombosis (PVT) may be as high as 13% in the first year or 20% overall in patients with tricuspid valve prosthesis and 0.2–6% patient per year in left-side prosthesis (1,2). Inadequate anticoagulation is the major contributing factor. Prosthetic vale thrombosis can present either as obstructive PVT or nonobstructive PVT. Acute obstruction leads to acute heart failure or cardiogenic shock or it can be an insidious process with acute thrombosis over pannus formation. Nonobstructive thrombosis may cause stroke or peripheral embolism but 50% may be asymptomatic. Guidelines differ on whether surgical treatment (reoperation or thrombectomy) or thrombolysis should be the treatment of choice since recommendations have largely been based on case reports or series with lack of well-designed prospective randomized trials. Thrombus size, NYHA functional class, contraindications, availability of each therapeutic option and the clinician’s experience are all likely determinants of outcome of prosthetic valve thrombosis.Surgery as the Traditional Management
The guidelines published by European Society of Cardiology (2007) and American College of Cardiology (2008)/American Heart Association (3) recommend surgery as reasonable first-line strategy for left-sided obstructive prosthetic valve thrombosis and thrombolysis reserved for specific situations like right-sided prosthetic thrombosis, lower functional NYHA class with small thrombus or when patient is in a higher NYHA class with large or small thrombus burden with a high operative risk. All recommendations are class II a or II b based on level B or C evidence. Reported operative mortality rates range between 0% and 69% depending on functional class and urgency of operation (2,4). Deveri et al. (5) reported a mortality of 4.7% even in patients with lower functional class (I or II). Valvular heart disease is more common in developing world along with high incidence of prosthetic thrombosis and access to urgent cardiac surgery is limited along with more patient refusals for surgery owing to high treatment costs and morbidity.
Thrombolysis as a Preferred Strategy
Surgery has been the traditional management of choice for obstructive PVT but recently thrombolysis has been proposed as first-line therapy due to high success rates with relatively low complication and mortality rates based on case reports/series with no randomized trials comparing thrombolysis and surgery for obstructive PHT.
Right-sided PVT
Thrombolysis has gained general acceptance for treatment of right-sided PVT because there is no risk of cerebral embolism and less complicated course of pulmonary embolism, which itself can be dealt with lytic therapy (6,7).
Left-sided prosthetic valve obstruction
Lengyel et al. (8) in 2005 recommended as a member of a Working Group of the Society of Heart Valve Disease that thrombolysis should be favored for almost all patients with PVT, with surgery reserved for those with contraindications to thrombolytic treatment or when thrombolysis has failed. Lengyel and Vandor (9) reported a case series of 59 patients (54 had obstructive PVT) over 7 years with 32 patients treated with thrombolysis. The success rates and mortality in thrombolytic group were 84.4% and 6.2%, respectively, as compared to 66.7% and 33.3% in surgical group.
In a single-center study of 127 patients, Roudant et al. (10) reported total dissolution of prosthetic valve associated thrombus in 71% patients and partial dissolution in 17%. Severe hemorrhagic complications were seen in 5% and systemic embolism in 15% causing cerebral infarction in only 7% of patients. All other transient ischemic attacks (TIAs) and peripheral embolism cases were managed with further antithrombotic therapy. Overall mortality with thrombolytic therapy was 12%. Failure of thrombolytic therapy was seen in 20% of patients. Earlier authors were concerned by high rates of systemic embolism associated with thrombolytic therapy; however this report showed that all embolic phenomena are minor and manageable with antithrombotic therapy. Alpert in an editorial comment (11) recommended that critical patient should be managed with thrombolytic therapy and a repeat thrombolysis can be administered based on serial echocardiographic monitoring. Patients who are stable that is in NYHA class I or II can be managed with either therapy. In a series of 68 patients (12) of PVT treated with fibrinolytic therapy, success was achieved in 91.2% of patients and failure was seen in 6 patients (8.8%). In NYHA class 4 patients, success rates were 88.9% with systemic embolism seen in only 5 patients.
A review paper by Caceres-Lorigaet et al. (13) also proposed thrombolytic therapy to be first-line strategy for obstructive PVT presenting with NYHA 3 or 4 symptoms or cardiogenic shock. Repeated infusions can also be given under echocardiographic guidance and surgery reserved for failure even after repeated thrombolysis. Stable patients with lower functional class can be managed with thrombolytic therapy or an antithrombotics depending on patient’s and the physician’s preference. Lengyel (14) published as a letter a meta-analysis of outcomes from thrombolysis for PVT, which included 53 studies and results were divided into the periods 1974–1995 and 1996–2003. This showed improved success rates (90%), embolic events (4%) and a mortality of only 2.5%.
The retrospective multicentric Prosthetic Valve Thrombolysis – Role of Transesophageal Echocardiogrphy (PRO-TEE) registry formed the basis for guidelines from American College of Chest Physicians (ACCP guidelines) (15). According to contributors of registry, thrombolysis should be reserved for patients with thrombus size of ≤0.8 cm2. Lengyel in a correspondence letter (14) argued that this conclusion was based on a small number of patients coming from 14 centers over 16 years. The selection of cases may have been biased. Moreover, in obstructive cases the fixed thrombus is difficult to be measured within the valve orifice. He concluded that thrombolysis should be considered irrespective of thrombus size and functional class.
In another series by Keuleer’s et al. (16), 31 patients with prosthetic valve thrombosis at a single center between 1988 and 2008 were treated with recombinant tissue plasminogen activator. Overall success rate was 92%. The only nonresponder was referred for surgery. Recurrence was seen in 31% patients over a follow-up of 18 months with 1 fatal event in a patient refusing further anticoagulation. Other complications were 1 stroke, 1 TIA and 2 peripheral embolism events with spontaneous resolution. Recurrent thrombosis after initial successful fibrinolysis, which is reported to occur in about 20% of patients, can also be managed with further thrombolytic therapy and anti-thrombotics. By a single-center study of 110 consecutive Indian patients, Gupta et al. (17) could establish no relation between the efficacy of thrombolytic therapy and functional class. They also observed a 70% success rate for rethrombolysis.
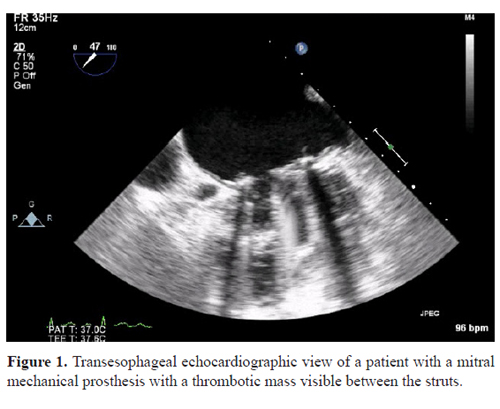
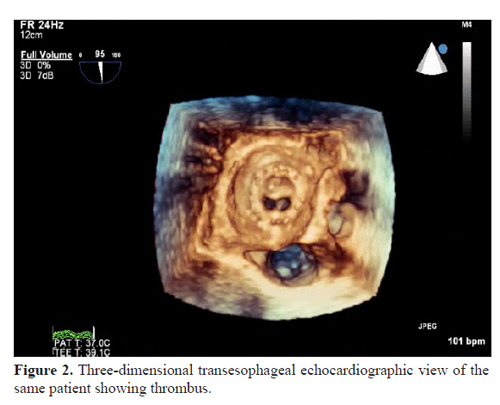
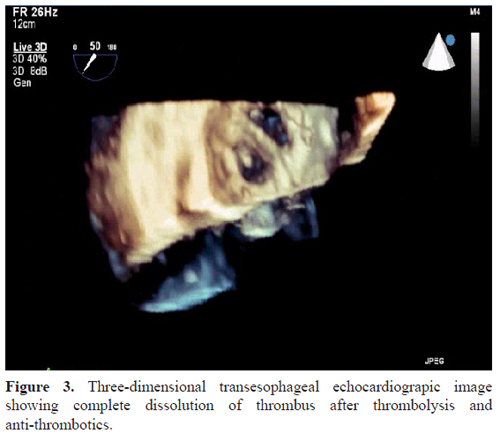
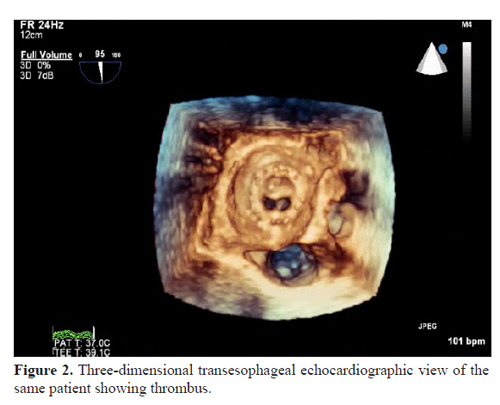
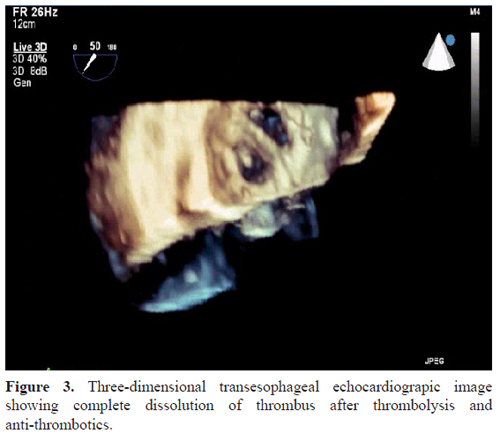
Figures 1–3 demonstrate 2D and 3D transesophageal echocardiographic images of a patient with a stuck mitral prosthesis with thrombus who was later successfully thrombolyzed at our center.
Complications with Thrombolytic Therapy – Do These Matter?
In a single-center study of 127 patients, Roudant et al. (10) reported total dissolution of prosthetic valve associated thrombus in 71% patients and partial dissolution in 17%. Severe hemorrhagic complications were seen in 5% and systemic embolism in 15% causing cerebral infarction in only 7% of patients. All other transient ischemic attacks (TIAs) and peripheral embolism cases were managed with further antithrombotic therapy. Overall mortality with thrombolytic therapy was 12%. Failure of thrombolytic therapy was seen in 20% of patients. Earlier authors were concerned by high rates of systemic embolism associated with thrombolytic therapy; however this report showed that all embolic phenomena are minor and manageable with antithrombotic therapy. Alpert in an editorial comment (11) recommended that critical patient should be managed with thrombolytic therapy and a repeat thrombolysis can be administered based on serial echocardiographic monitoring. Patients who are stable that is in NYHA class I or II can be managed with either therapy. In a series of 68 patients (12) of PVT treated with fibrinolytic therapy, success was achieved in 91.2% of patients and failure was seen in 6 patients (8.8%). In NYHA class 4 patients, success rates were 88.9% with systemic embolism seen in only 5 patients.
A review paper by Caceres-Lorigaet et al. (13) also proposed thrombolytic therapy to be first-line strategy for obstructive PVT presenting with NYHA 3 or 4 symptoms or cardiogenic shock. Repeated infusions can also be given under echocardiographic guidance and surgery reserved for failure even after repeated thrombolysis. Stable patients with lower functional class can be managed with thrombolytic therapy or an antithrombotics depending on patient’s and the physician’s preference. Lengyel (14) published as a letter a meta-analysis of outcomes from thrombolysis for PVT, which included 53 studies and results were divided into the periods 1974–1995 and 1996–2003. This showed improved success rates (90%), embolic events (4%) and a mortality of only 2.5%.
The retrospective multicentric Prosthetic Valve Thrombolysis – Role of Transesophageal Echocardiogrphy (PRO-TEE) registry formed the basis for guidelines from American College of Chest Physicians (ACCP guidelines) (15). According to contributors of registry, thrombolysis should be reserved for patients with thrombus size of ≤0.8 cm2. Lengyel in a correspondence letter (14) argued that this conclusion was based on a small number of patients coming from 14 centers over 16 years. The selection of cases may have been biased. Moreover, in obstructive cases the fixed thrombus is difficult to be measured within the valve orifice. He concluded that thrombolysis should be considered irrespective of thrombus size and functional class.
In another series by Keuleer’s et al. (16), 31 patients with prosthetic valve thrombosis at a single center between 1988 and 2008 were treated with recombinant tissue plasminogen activator. Overall success rate was 92%. The only nonresponder was referred for surgery. Recurrence was seen in 31% patients over a follow-up of 18 months with 1 fatal event in a patient refusing further anticoagulation. Other complications were 1 stroke, 1 TIA and 2 peripheral embolism events with spontaneous resolution. Recurrent thrombosis after initial successful fibrinolysis, which is reported to occur in about 20% of patients, can also be managed with further thrombolytic therapy and anti-thrombotics. By a single-center study of 110 consecutive Indian patients, Gupta et al. (17) could establish no relation between the efficacy of thrombolytic therapy and functional class. They also observed a 70% success rate for rethrombolysis.
Figures 1–3 demonstrate 2D and 3D transesophageal echocardiographic images of a patient with a stuck mitral prosthesis with thrombus who was later successfully thrombolyzed at our center.
Prosthetic Valve Thrombosis in Pregnancy
Experience regarding thrombolytic therapy in pregnant patients with prosthetic heart valve (PHV) thrombosis is limited. There have been several case reports where pregnant patients with prosthetic valve thrombosis were thrombolyzed successfully (18). First large-scaled study TROIA-PREG presented at ESC Congress 2012 (Beytullah CAKAL), conducted in pregnant patients with prosthetic valve thrombosis who underwent thrombolytic therapy with low dose, slow infusion of rt-tPA with repetition as needed, resulted in 100% success rates with spontaneous abortion rates of 14.8%, which is comparable to that in pregnant patients with PHVs (19.1%). Hence, thrombolytic therapy can be considered as a first-line therapy in pregnant patients with PHV thrombosis.
Failure of Thrombolytic Therapy or Partial Response
As very clear from previous discussion, thrombolytic treatment failure or partial response does not preclude surgery. It is possible to perform early surgery once thrombolytic agent has been neutralized and it leads to better hemodynamic status of the patient before surgery (rescue fibrinolysis). Early post-operative thrombolytic therapy has been reported as early as 4 days after valve replacement without complications (19). Reddy et al. (20) noted that 43% of patients with partial improvement after thrombolytic therapy demonstrated eventual complete restoration of valve mobility after 3–12 months of observation and anticoagulation. They reported a mortality of 18% in patients requiring surgery after thrombolytic failure, which is almost comparable or even lower than that reported with primary surgery cases in different case series.
Complications with Thrombolytic Therapy – Do These Matter?
Clinical complications due to thrombolysis tend to be minor and reversible. Minor bleeding complications can be treated with local hemostatic measures. In case of major bleedings, fibrinolytic effect can be reversed with fresh frozen plasma infusions and protease inhibitors. Moreover, with the availability of newer generation thrombolytic agents and use of slow infusion of these agents especially rt-tPA at low dose (25 mg), slow infusion over 6 hours has resulted in lower bleeding complications and thromboembolism (21). Peripheral embolic phenomenon can be managed with thrombolysis itself or anti-thrombotics. Thrombolytic therapy has also been recommended during early stages of ischemic stroke (22).
Cost-effectiveness and availability
Thrombolysis is certainly more cost-effective than re-operation, which is an important consideration in developing countries where a substantial number of patients cannot afford a second operation (23). Thrombolytic drugs are easily available at any medical facility as compared to emergency surgery, which is not available at all places at all times especially in developing countries (24). Till date there are no prospective randomized trials comparing the two modalities. A single-center, prospective study from India named SAFE-PVT (Surgery versus Thrombolytic Therapy for Left-sided Prosthetic Valve Thrombosis) will be conducted over 4 years to compare thrombolysis and surgery in terms of efficacy, safety and cost-effectiveness of each treatment.
Summary
Prosthetic valve obstruction with thrombus is an emergency condition with rapid hemodynamic deterioration with high mortality and warrants immediate management. Because of lack of prospective randomized trials comparing surgery and thrombolysis, first-line therapy remains controversial. More recent data have shown thrombolysis to be superior to surgery in terms of high success rates, low mortality, ease of administration, cost-effectiveness, availability, patient’s preference and easily manageable complications (Tables 1 and 2). It does not contraindicate surgery if there is no or partial response. Surgery should be reserved for thrombolytic failure cases and when absolute contraindications exist as for other indications of fibrinolysis. Thrombolysis offers an effective and reliably safe nonsurgical treatment of prosthetic valve obstruction irrespective of thrombus size or functional class and should be considered as first-line therapy in majority of patients. The recent data calls for new consensus guidelines regarding management of prosthetic vale occlusion.
.jpg)
.jpg)
References
.jpg)
.jpg)
References
- Roudaut R, Labbbe T, Lorient-Roudaut M-R. Mechanical cardiac valve thrombosis: is thrombolysis justified? Circulation. 1992; 86 (Suppl 2):8–15.
- Lengyel M, Fuster V, Keltai M, Roudaut R, Schulte HD, Sewar JB, Chesebro JH, Turpie AGG. Guidelines for management of left-sided prosthetic valve thrombosis: a role of thrombolytic therapy. J Am Coll Cardiol. 1997; 30:1521–6.
- American College of Cardiology/American Heart Association Task Force on Practice Guidelines; Society of Cardiovascular Anesthesiologists; Society for Cardiovascular Angiography and Interventions; Society of Thoracic Surgeons, Bonow RO, Carabello BA, Kanu C, de Leon AC, Jr, Faxon DP, Freed MD, Gaasch WH, Lytle BW, Nishimura RA, O’Gara PT, O’Rourke RA, Otto CM, Shah PM, Shanewise JS, Smith SC, Jr, Jacobs AK, Adams CD, Anderson JL, Antman EM, Faxon DP, Fuster V, Halperin JL, Hiratzka LF, Hunt SA, Lytle BW, Nishimura R, Page RL, Riegel B. ACC/AHA 2006 guidelines for the management of patients with valvular heart disease. Circulation. 2006; 114:e84–231.
- Horstkotte D, Burckhardt D. Prosthetic valve thrombosis. J Heart Valve Dis. 1995; 4:141–53.
- Deviri E, Sareli P, Wisenbaugh T, Cronje SL. Obstruction of mechanical heart valve prosthesis: clinical aspects and surgical management. J Am Coll Cardiol. 1991; 17:646–50.
- Shapira Y, Sagie A, Jortner R, Adler Y, Hirsh R. Thrombosis of bileaflet tricuspid valve thrombosis: clinical spectrum and role of non-surgical treatment. Am Heart J. 1999; 137:721–5.
- Villanyi J, Wladika ZS, Bartek I, Lengyel M. Diagnosis and treatment of tricuspid mechanical prosthetic valve dysfunction [abstract]. Eur Heart J. 1992; 13(Suppl):374.
- Lengyel M, Horstkotte D, Voller H, Mistiaen WP. Working group Infection, Thrombosis, Embolism and Bleeding of the Society for Heart Valve Disease. Recommendations for the management of prosthetic valve thrombosis. J Heart Valve Dis. 2005; 14:567–75.
- Lengyel M, Vandor L. The role of thrombolysis in management of left sided prosthetic valve thrombosis: a study of 85 cases diagnosed by transesophageal echocardiography. J Heart Valve Dis. 2001; 10:636–49.
- Roudaut R, Lafitte S, Roudaut MF, Courtault, Perron JM, Jais C, Pillois X, Coste P, DeMaria A. Fibrinolysis of mechanical prosthetic valve thrombosis: a single centre study of 127 cases. J Am Coll Cardiol. 2003; 41:653–8.
- Alpert SJ. The thrombosed prosthetic valve (Editorial). J Am Coll Cardiol. 2003; 41,4:659–60.
- Cáceres-Lóriga FM, Pérez-López H, Morlans-Hernández K, Facundo-Sánchez H, Santos-Gracia J, Valiente-Mustelier J, Rodiles-Aldana F, Marrero-Mirayaga MA, Betancourt BY, López-Saura P. Thrombolysis as a first choice therapy in prosthetic heart valve thrombosis. A study of 68 patients. J Thromb Thrombolysis. 2006; 21:185–90.
- Caceras-Loriga FM, Perez-Lopez H, Sanotz-Gracia J, Monlans-Hernandez K. Prosthetic heart valve thrombosis: pathogenesis, diagnosis and management. Int J Cardiol. 2006; 110:1–6.
- Lenegyel M. Thrombolysis should be regarded as a first line therapy for prosthetic valve thrombosis in absence of contraindications. J Am Coll Cardiol. 2005; 45(2):325 (Letter).
- Tong TA, Roudaut R, Ozkan M, Sagie A, Shahid MS, Pontes SC, Jr, Carreras F, Girard SE, Arnout S, Stainback RF, Thadhani R, Zogbhi WA. Prosthetic valve thrombosis – role of transesophageal echocardiography. Tranesophageal echocardiography improves risk assessment of thrombolysis of prosthetic valve thrombosis: results of international PRO-TEE registry. J Am Coll Cardiol. 2004; 43:77–84.
- Keuleers S, Heijjegers P, Herregods MC, Budts W, Dubois C, Meuris B, Verhamme P, Flameng W, Van de Werf F, Adriaenssens T. Comparison of thrombolysis and surgery as a first line therapy for prosthetic heart valve thrombosis. Am J Cardiol. 2011; 107(2):275–9.
- Gupta D, Kothari SS, Bahl VK, Goswami KC, Manchanda SC, Venugopal P. Thrombolytic therapy for prosthetic valve thrombosis: short and long-term results. Am Heart J. 2000; 140:906–16.
- Sriniwas BC, Moorthy N, Kuldeep A, JeevanH, Chandrasekaran D, Manjunath CN. Thrombolytic therapy in prosthetic valve thrombosis during early pregnancy. Indian Heart J. 2012; 64(1):74–6.
- Lengyel M. Management of prosthetic valve thrombosis. J Heart Valve Dis. 2004; 13:329–34.
- Reddy NK, Padmanabhan TN, Singh S, Kumar DN, Raju PR, Satyanarayana PV, Rao DP, Rajgopal P, Raju BS. Thrombolysis in left-sided prosthetic valve occlusion: immediate and follow-up results. Ann Thorac Surg. 1994; 58:462–71.
- Bonou M, Lampropolous K, Barbetseas J. Prosthetic heart valve obstruction: thrombolysis or surgical treatment? Eur Heart J: Acute Cardivascular Care. 2012; 1:122–7.
- Lawrence R. Intravenous thrombolytic therapy for acute ischaemic stroke. N Engl J Med. 2011; 364:2138–46.
- Ganeasan K, Bhima S, Mathew RS, Mathew N, Kalaivani M, Singh S, Bahl VK, Hirsh J, Eikelboom JW. Accelerated infusion of streptokinase for treatment of left-sided prosthetic valve thrombosis. A randomized controlled trial. Circulation. 2009; 120:1108–14.
- Cacera-Loriga FM. Prosthetic valve thrombosis: is it time for a new consensus conference (Guest Editorial). Eur J Echocardiography. 2008; 9:413–4.
- Why Publish with JCPC?
- Instructions to the Authors
- Submit Manuscript
- Advertise with Us
- Journal Scientific Committee
- Editorial Policy
Print: ISSN: 2250-3528


