The Journal of Clinical and Preventive Cardiology has moved to a new website. You are currently visiting the old
website of the journal. To access the latest content, please visit www.jcpconline.org.
Original Article
Prevalence of Metabolic Syndrome in Prehypertensive Urban Adult Population
Volume 4, Jan 2015
Om Murti Anil, Kathmandu, Nepal
J Clin Prev Cardiol. 2015;4(1):1-6
The metabolic syndrome (MS) is a constellation of interrelated risk factors of metabolic origin (1). Although dietary habits, demographic characteristics have been associated with MS; body mass index (BMI), weight gain and physical inactivity are the most important risk factors for the development of this syndrome. Basic defect in this syndrome is insulin resistance, which is considered to be related with abdominal adiposity, physical inactivity, impaired fasting glucose, impaired glucose tolerance; type 2 diabetes, cardiovascular disease and overall mortality.Metabolic syndrome is emerging as a global epidemic. Prevalence of this syndrome is age dependent. According to Third National Health and Nutrition Examination Survey (NANHES III), 24% of US adults had the MS ABSTRACTbased on the ATP III criteria. Prevalence of this syndrome is 7% among adult aged 20 to 29 years and rises to 40% or more among elderly above 60 years (2).
Metabolic syndrome is associated with development of cardiovascular disease. It is associated with four fold increase in risk of fatal coronary heart disease and two fold greater risk of cardiovascular disease and all causes of mortality among men; even after adjusting for age, LDL-C, diabetes, smoking and family history of coronary heart disease (CHD). It is also an important predictor of type 2 diabetes. Patients with MS have 5 to 9 fold increase risk of developing type 2 diabetes (3).
Prehypertension has been described as an independent category of blood pressure (BP). Prehypertension, defined by JNC (Joint National Committee), as systolic BP 120-139 mmHg and/or diastolic BP 80-89 mmHg, is associated with lower insulin sensitivity (4). According to the recent result to the Third National Health and Nutrition Examination Survey, prehypertension is present in 31% of adults in the United States, and this condition is associated with an increased prevalence of both heart disease and risk for stroke (3). National Cholesterol Education Program/ Adult Treatment Panel III (NCEP/ATPIII 2001) and International Diabetes Federation (IDF 2005) have given simple and easily applicable criteria for the diagnosis of metabolic syndrome. In 2005, IDF has proposed a worldwide definition especially focusing different ethnicity across the world (5).
In the above context, detecting MS in prehypertensive and hypertensive individuals becomes important for both preventing and treating hypertension, type 2 diabetes and other cardiovascular disorders. There have been large number of studies conducted across the world about prevalence, risk factors and treatment of MS but there are very few studies conducted on prevalence of metabolic syndrome among prehypertensive individuals.
Detecting the MS by IDF 2005 definition is more applicable in Asian countries, like Nepal. Till date, to the best of authors’ knowledge, only few studies have been conducted on this subject in Nepal but no data is available regarding prevalence of prehypertension in the country. This study aims on showing the difference in prevalence of MS among prehypertensive and hypertensive participants and also compares the prevalence of MS identified by earlier (ATPIII) and recent (IDF) definitions.
Materials and Methods
Materials and Methods
It was a descriptive analytical cross-sectional study, which was conducted among healthy adults of Kathmandu attending a heart disease prevention awareness camp in the month of September 2014. Consecutive 50 male and 50 female participants were selected in this study for each of the three groups; namely normotension, prehypertension and hypertension. Although study population was taken from group of people attending a free heart camp, they were randomly grouped into three categories (normotensive, prehypertensive and hypertensive groups), which eliminated opportunistic screening as well as selection bias.
Altogether 300 participants (150 male and 150 female) were enrolled after carefully applying the inclusion and exclusion criteria.
Inclusion Criteria
Blood Pressure was recorded by same instrument in sitting position in right and left arm after 5 minutes of rest in sitting position with standard protocol. A minimum of three readings were taken and a mean value of all measurement was taken. Weight was recorded by same weighing machine and nearest value in 0.5 kg was taken. Abdominal circumference was measured from highest point of iliac crest while participant is talking minimal respiration. Nearest value in 1 cm was recorded. Hip circumference was measured from widest part of hip in nearest 1 cm. Height was measured in nearest 1 cm. We also took a 12 hour fasting blood sample for measurement of blood sugar and blood lipid level. Biochemical analysis of blood done within international standard and protocol in same laboratory and all the lipid parameters were measured.
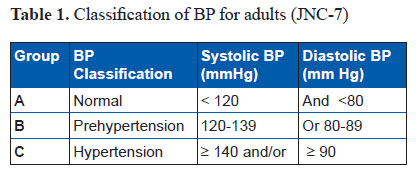
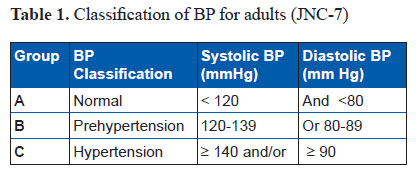
All the participants were divided into 3 groups according to the Seventh Report of the Joint National Committee (JNC) on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (Table 1).
References
- Age 18 years and above
- Performs normal daily activity
- Gives consent for the research
- Pregnant women
- Participants having any acute systemic illness.For e.g. infectious, inflammatory, acute coronary event, acute cerebrovascular accident.
- Diseases known to alter blood sugar and lipid. For e.g. chronic liver or kidney disease.
- Known case of hypertension, diabetes or dyslipidemia
- Participants already on drugs known to alter BP, blood sugar and blood lipid level.
Blood Pressure was recorded by same instrument in sitting position in right and left arm after 5 minutes of rest in sitting position with standard protocol. A minimum of three readings were taken and a mean value of all measurement was taken. Weight was recorded by same weighing machine and nearest value in 0.5 kg was taken. Abdominal circumference was measured from highest point of iliac crest while participant is talking minimal respiration. Nearest value in 1 cm was recorded. Hip circumference was measured from widest part of hip in nearest 1 cm. Height was measured in nearest 1 cm. We also took a 12 hour fasting blood sample for measurement of blood sugar and blood lipid level. Biochemical analysis of blood done within international standard and protocol in same laboratory and all the lipid parameters were measured.
All the participants were divided into 3 groups according to the Seventh Report of the Joint National Committee (JNC) on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (Table 1).
Diagnosis
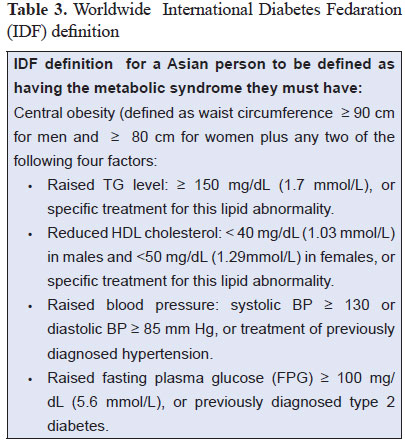
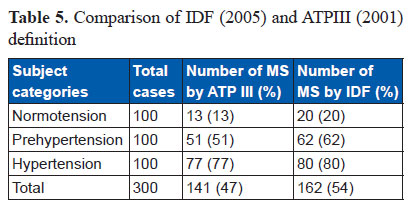
Metabolic Syndrome was diagnosed on the basis of two different criteria given by NCEP/ATPIII 2001 as mentioned in Table 2 and IDF 2005 as mentioned in Table 3. The NCEP/ATP III criteria required presence of 3 of 5 factors as the basis for establishing the diagnosis (1).

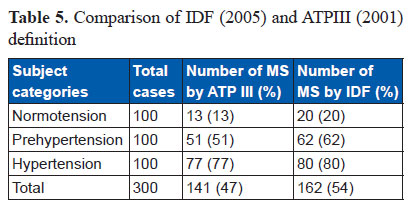
Prevalence of the metabolic syndrome in this study was 54 % (162 of 300 subjects) by International Diabetes Federation 2005 (IDF) criteria while prevalence by Adult Treatment Panel III 2001 (ATPIII) criteria was 47 % (141 of 300 subjects) (Table 5).
This study provides a look at prevalence of the metabolic syndrome in a cohort of urban adult Nepalese population by using both IDF and NCEP/ATP III criteria. In IDF criteria, using the IDF definition, the prevalence of the MS was 54.2% (men 50%; women 58.3%). In comparison, prevalence of the metabolic syndrome defined according to NCEP/ATP III 2001 criteria were 47.5% (men 41.7%; women 53.3%). This clearly showed that IDF definition estimates higher prevalence of metabolic syndrome than ATP III criteria.

Statistical Analysis
Data were entered on the computer by using the SPSS Statistical Software (Version 20; SPSS; Chicago, IL) and were analyzed on the same software. Quantitative variables are presented as mean (+ standard deviation). One-way analysis of variance (ANOVA) and the and χ2 test were used to analyze the statistical differences among characteristics of participants, and one-way ANOVA was applied to compare the three categories of BP. Wherever applicable, the data were presented using both the tabular method and descriptive statistics. P value <0.05 was considered statistically significant.
Results
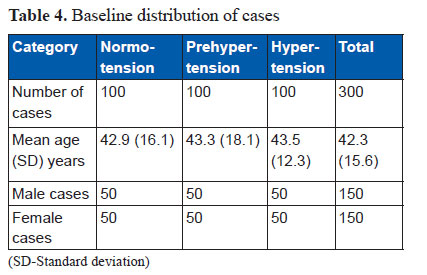
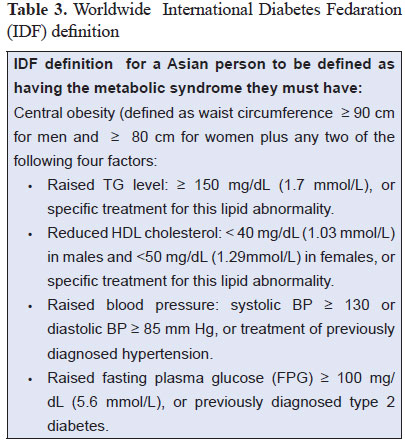
Altogether 300 eligible participants, divided into three equal groups i.e. Normotension; Prehypertension and hypertension, were included in this study. There were 50 male and 50 female participants in each of the three groups (Table 4). Mean age of all the participants was 42.3+15.6 years. The mean age of male participants was 42.4+16.9 years and that of female participants was 42.2+16.9 years (Table 4).
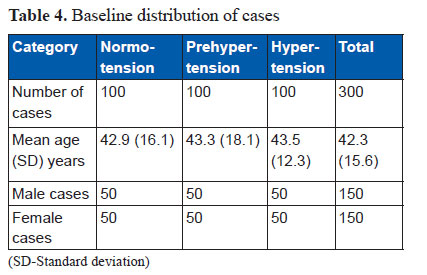
Prevalence of the metabolic syndrome in this study was 54 % (162 of 300 subjects) by International Diabetes Federation 2005 (IDF) criteria while prevalence by Adult Treatment Panel III 2001 (ATPIII) criteria was 47 % (141 of 300 subjects) (Table 5).
Out of 162 cases of MS, 76 were male and 86 female accounting 47% and 53% respectively. Prevalence of MS was 50% (76 out of 150) in male population and 57.3% (86 out of 150) in female population. It was lowest in 18-39 age group (30%) and highest in 50 years and above age group (72.7%). There was a clear age-related increase in the prevalence of the metabolic syndrome in this population. Prevalence was higher in elderly age group than in younger individuals. In less than 50 age group, prevalence was 43.4%, while that in 50 and above age group it was 72.7%.
Metabolic syndrome was twice more common in hypertensive than non-hypertensive (41% vs. 80%). Not a single case of MS was found in individuals with BMI less than 20 kg/m2; on the other hand, prevalence was very high in group with BMI ≥ 25 kg/m2 (92.5%).
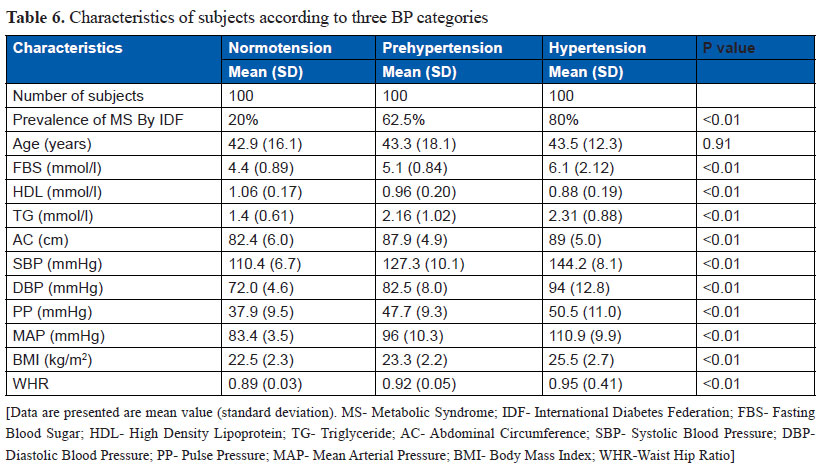
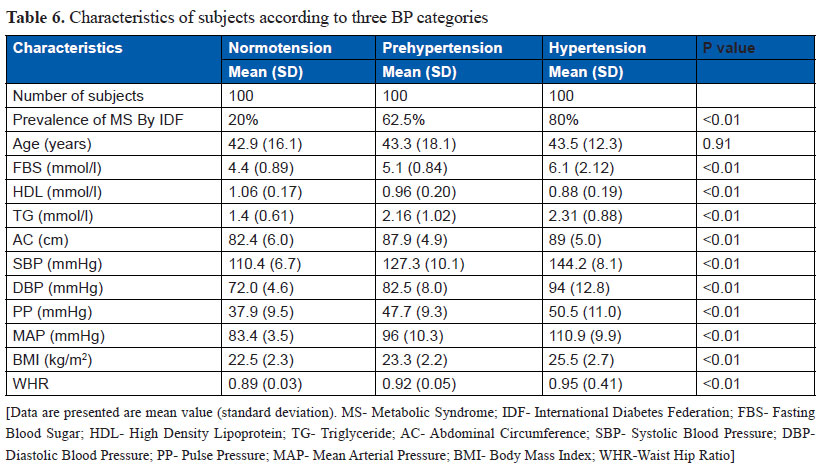
Prevalence of MS by IDF criteria was highest among hypertensive group (80%), followed by prehypertensive (62.5%) and normotensive groups (20%). The difference among the three groups regarding the prevalence of MS was statistically significant (P value < 0.01). When we applied ATP III criteria, prevalence of MS decreased to 77.55%, 52.5% and 12.5% in hypertensive, prehypertensive and normotensive individuals, respectively.
The values for fasting blood sugar, triglyceride, abdominal circumference, waist hip ratio, BMI and BP (systolic, diastolic, pulse and mean) was highest among hypertensive; intermediate among prehypertensive and lowest among normotensive group. Similarly, level of HDL was lowest in hypertensive and highest in normotensive, while prehypertensive group showed intermediate level. The difference among three groups remained statistically significant for all variables mentioned above (Table 6).
Discussion
Study done by Sharma et al. (6) in eastern part of Nepal showed 22.5% of the participants had MS based on IDF criteria and 20.7% according to the NCEP definition. Similarly, another study done by Bhattarai S et al. (7) in western part of Nepal showed prevalence of MS in diabetes patients as per NCEP/ATP III and IDF criteria 71% and 82%, respectively. Prevalence of MS in US adult was 26.7% (male 23.3% and female 29.3%) in NHANES8 1999-2000 study.
With the most recent national data from US adults and the definition of the metabolic syndrome proposed by the IDF, almost 40% of US adults (male 39.9% and female 38.1%) were classified as having the MS, a prevalence that is higher than that estimated by the NCEP definition (34.5%) (male 33.7% and female 35.4%). In the same study, prevalence of MS in Mexican-American men was 40.3% (by ATPIII) and 50.6% (by IDF) (9).
According to Sobhanjan Sarkar et al., in India, it was seen that the presence of MS was alarmingly high (approximately 30-50%) among both the rural and the urban Bhutia population. Further, the prevalence was higher among females (about 50%) than among males (about 28%); by NCEP/ATP III 2001 criteria (10).
The above mentioned studies have shown the prevalence of MS ranging from 24- 45% by NCEP/ATP III criteria and 42.5- 50% by IDF criteria. In our cohort, prevalence is slightly higher (54.2%) than above range. This slight higher prevalence in this study is due to lower abdominal obesity criteria for Asians in IDF criteria. Prevalence of MS is higher in females than males and most of the studies mentioned above support this difference (10). Prevalence of MS in our study was higher in females (58%) than in males (50%).
Prevalence of MS increases with age and there is a linear relationship between these two. Most of the studies done on this subject show this relationship. Alberto Cordero et al. showed that prevalence of MS increased with respect to age. P value< 0.01 within all age group (4). In this study, prevalence of MS increased with respect to age (P value < 0.01).
The most important and largest study conducted in prehypertensive population was the MESYAS Registry substudy (4). This study prospectively collected 19,041 healthy active workers with mean age of 42.2 (10.7) years. Presence of MS was assessed according to the modified criteria of the NCEP/ATP III. The global presence of MS was 11.8%. A higher prevalence was found in subjects with hypertension (30%), followed by those with prehypertension (9.6%). The prevalence of MS in above three BP categories were statistically significant (P value < 0.01).
The global prevalence of MS in this population is lower than in other published cohorts. Nonetheless, the important finding is not the absolute value of prevalence but rather the differences in the prevalence and metabolic profiles among the three categories of BP. This population is strictly constituted by active workers without overt daily-life-limiting diseases and ATP III criteria were applied for diagnosis of MS.
In our study, prevalence of MS by IDF criteria was highest among hypertensive group (80%), followed by prehypertensive (62.5%) and normotensive (20%). When we applied ATPIII criteria, prevalence of MS decreased to 77.5%, 52.5% and 12.5% in hypertensive, prehypertensive and normotensive individuals, respectively. The reason for higher prevalence of MS in our cohort has already been explained. The most important aspect was the difference in prevalence between the three BP category, which is highly significant (P value < 0.01).
According recent data from US, prevalence of MS is twice more common in hypertensives than in nonhypertensives. In hypertensive individuals, prevalence was 62.9 ± 3.3% and that in nonhypertensives was 25 ± 2% by IDF criteria (9). Prevalence of the MS in the Spanish hypertensive population was 44.6% by using NCEP criteria and 61.7% when IDF criteria were applied (11).
Limitations of the Study
The participants enrolled in this study were selected from those attending a free heart camp and these participants may not represent similar characteristics that of entire community or population. Therefore results obtained from this study may not reflect the exact situation of population of a community or the country.
Conclusions
Metabolic syndrome is a very common condition and its prevalence is increasing. In this selected Nepalese population also, prevalence is very high (54%). IDF definition estimates higher prevalence of MS than ATP III criteria (54.2% Vs 47.5%) due to difference in obesity criteria and lower threshold used for impaired fasting glucose. Prehypertension is associated with marked increase in prevalence of MS compared to normotension. This explains that prehypertension is an insulin resistance state. Prevalence of MS is highest in hypertensive (80%) individuals as compared to prehypertensives and normotensives. Metabolic syndrome is more common in females, elderly, hypertensives and obese individuals.
Components of MS are interdependent, but each component is indirectly linked with unhealthy lifestyle and emergence of this syndrome. This study didn’t aim to show the relationship between MS and its components.
Higher prevalence of this syndrome in prehypertensive individuals will further reinforce the importance of lifestyle changes not only in prevention of development of hypertension but also cardiovascular disease and its related complications.
Above all, this study was conducted in Kathmandu valley, which represents people from various regions of Nepal including mountains and Himalayas. Prevalence of MS in this cohort of population will provide a new look on Southeast Asians residing at higher altitude.
References
- National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (Adult treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report Circulation. 2002; 106:3143-421.
- Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: findings from the Third National Health and Nutrition Examination Survey. JAMA 2002;287:356-9.
- Chobanian AV, Bakris GL, Black HR et al. National Heart, Lung and Blood Institute Joint National Committee on Prevention, Detection , Evaluation and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The seventh Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure: the JNC 7 report. JAMA.2003;289:2560-2572.
- Cordero A, Laclaustra M, León M, Grima A, Casasnovas JA, Luengo E, del Rio A, Ferreira I, Alegria E.. Prehypertension is associated with insulin resistance state and not with an initial renal function impairment. A Metabolic Syndrome in Active Subjects in Spain (MESYAS) Registry Substudy. Am J Hypertens 2006; 19:189-196.
- International Diabetes Federation. Worldwide definition of the metabolic syndrome . Available at: http://www.idf.org/webdata/docs/IDF_Metasyndrome_definition.pdf.
- Sharma SK, Ghimire A, Radhakrishnan J, Thapa L, Shrestha NR, Paudel N, Gurung K, R M, Budathoki A, Baral N, Brodie D. Prevalence of Hypertension, Obesity, Diabetes, and Metabolic Syndrome in Nepal. Int J Hypertens. 2011;2011:821971.
- Bhattarai S, Kohli SC, Sapkota S. Prevalence of metabolic syndrome in type 2 diabetes mellitus patients using NCEP/ATP III and IDF criteria in Nepal. Nepal J Med Sci. 2012;1:79–83.
- Ford ES, Giles WH. Increasing prevalence of the metabolic syndrome among U.S. adults. Diabetes Care 2004;27:2444-9.
- Ford ES. Prevalence of the metabolic syndrome defined by the International Diabetes Federation among adults in the U.S. Diabetes Care 2005;28:2745-9.
- Sarkar S, Das M, Mukhopadhyay B, Chakrabarti CS, Majumder PP.. High prevalence of metabolic syndrome and its correlates in two tribal populations of India & the impact of urbanization. Indian J Med Res. 2006;123:679-86.
- de la Sierra A, Romero R, Bonet J, Pérez M, López JS, Ravella R, Aguilera MT; Investigadores del estudio ESOPOH.. Prevalence and general features of the metabolic syndrome in the Spanish hypertensive population. Med Clin (Barc). 2006;126:406-9.
- Why Publish with JCPC?
- Instructions to the Authors
- Submit Manuscript
- Advertise with Us
- Journal Scientific Committee
- Editorial Policy
Print: ISSN: 2250-3528


