The Journal of Clinical and Preventive Cardiology has moved to a new website. You are currently visiting the old
website of the journal. To access the latest content, please visit www.jcpconline.org.
Student's Page
Is it a Pacemaker or a Defibrillator? Understanding Cardiovascular Implantable Electronic Devices
Volume 2, Apr 2013
Kartikeya Bhargava MD, DNB, Gurgaon, India
J Clin Prev Cardiol 2013;2(2):108-12
Cardiovascular implantable electronic devices (CIED) refers to electronic devices that are implanted in the patient’s body for diagnosis or treatment of patients with heart rhythm disorders or heart failure.
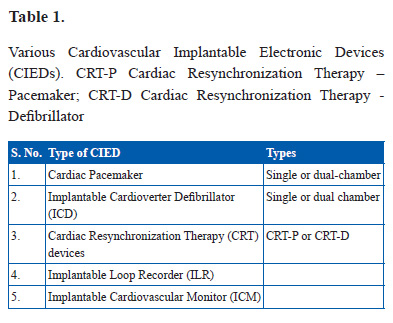
These various CIEDs are listed in Table 1.
All these devices can be interrogated using an instrument known as programmer that is specific to the device company. During interrogation the various device functions can be tested, the status of the battery can be known, stored diagnostic data including intracardiac electrograms of the episodes can be retrieved for evaluation and finally the device parameter settings can be altered as per need.
Often a patient has been implanted with an ICD, though the patient, his relatives and even his family physician think and repeatedly refer to the patient as having a pacemaker. To clarify these issues, the current article describes the basic features of these devices, including its uses and the ways to differentiate especially on chest X-ray.
Various types of CIEDs
Thus, it is clear that not all implantable electronic devices are pacemakers and it is of paramount importance for not only physicians & radiologists but also patients & their relatives to understand what kind of CIED a person has. A chest X-ray can not only help in identifying the type of device but also ascertain the device company by special radiological markers present on the device. Of course, it will help in detection of complications like lead dislodgement or fracture and device migration.
All these devices can be interrogated using an instrument known as programmer that is specific to the device company. During interrogation the various device functions can be tested, the status of the battery can be known, stored diagnostic data including intracardiac electrograms of the episodes can be retrieved for evaluation and finally the device parameter settings can be altered as per need.
Often a patient has been implanted with an ICD, though the patient, his relatives and even his family physician think and repeatedly refer to the patient as having a pacemaker. To clarify these issues, the current article describes the basic features of these devices, including its uses and the ways to differentiate especially on chest X-ray.
Various types of CIEDs
- Cardiac Pacemaker - A permanent cardiac pacemaker is an electronic device that is used to maintain adequate heart rate in patients with slow heart rhythm disorder or bradyarrhythmias. The components of a pacemaker system include –
- Pulse generator – A pulse generator is implanted in a subcutaneous or submuscular pocket usually in infraclavicular region and consists of a battery, a sensing amplifier that processes the sensed intrinsic beats, the computer software for pacemaker and an output circuitry that delivers timed electrical impulses to various heart chambers through the connected leads. The pulse generator of the pacemaker is a sealed device with an outer casing of titanium.
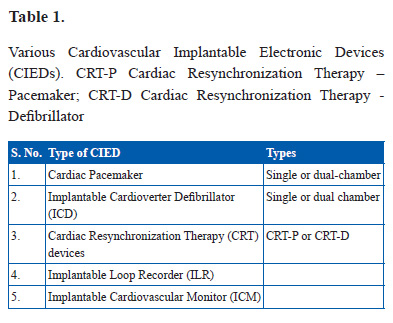
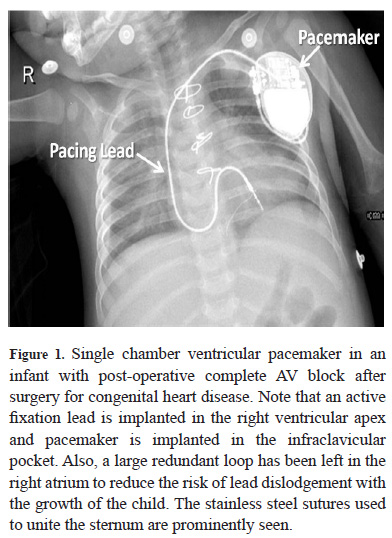
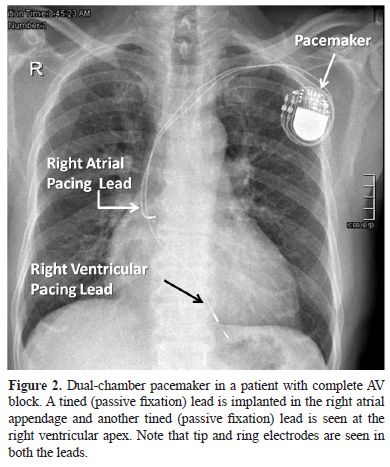
- Pacing leads – the pacing leads are implanted in the atrium and/or the ventricle through an access in the subclavian or axillary vein and connect the endocardial surface of the heart to the pulse generator. Commonly used bipolar leads have two electrodes – one at the tip and another close to the tip known as the ring electrode. These tip and ring electrodes are involved in the circuit that senses and paces the cardiac chamber. The pacing lead may have either passive fixation mechanism (tined lead) or active fixation mechanism (screw-in lead). (Figures 1 and 2)
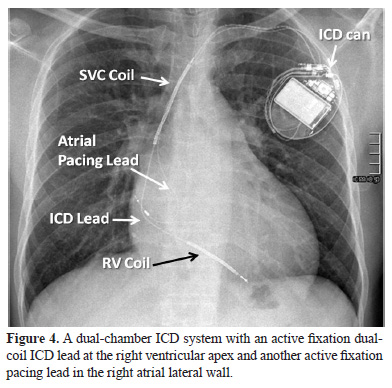
The pacemaker is implanted in patients who have symptoms related to slow heart rate or dangerously slow heart rhythm in the absence of symptoms. These occur either due to problem in natural pacemaker (sino-atrial node) or conduction of impulses from the atria to the ventricles – AV block. The pacemaker is of two types – single chamber pacemaker – has a single lead either in the atrium or in the ventricle (Figure 1) and dual-chamber pacemaker – has two leads – one in the atrium and another in the ventricle (Figure 2). The atrial lead is implanted in the right atrial appendage (Figure 2) or the right atrial lateral wall (Figure 4). The ventricular lead s usually implanted at the right ventricular apex (Figure 2) or in the right ventricular outflow tract or mid septum.
The pacemaker aims to maintain adequate heart rate at rest and also during exercise (rateresponsive pacing). It is designed to stimulate theatrium and/or the ventricle in the absence of a sensed intrinsic activity in the respective chamberso as to simulate a normal cardiac rhythm. If the patient’s intrinsic heart rate becomes high (tachycardia) a usual pacemaker cannot do anything to treat that and simply remains inhibited.
- Pulse generator – A pulse generator is implanted in a subcutaneous or submuscular pocket usually in infraclavicular region and consists of a battery, a sensing amplifier that processes the sensed intrinsic beats, the computer software for pacemaker and an output circuitry that delivers timed electrical impulses to various heart chambers through the connected leads. The pulse generator of the pacemaker is a sealed device with an outer casing of titanium.
- Implantable Cardioverter Defibrillator (ICD) – An ICD is an electronic device that is meant to automatically treat fast heart rhythms arising from the ventricles (ventricular tachycardia or fibrillation) by delivering a shock. Hence, it prevents sudden death due to ventricular tachyarrhythmias and isimplanted in patients who have already survived an episode of these arrhythmias (secondary prevention) or in patients who have never had these arrhythmias but are at a very high risk of having them due to theirunderlying cardiac disorder (primary prevention).
The components of an ICD include –
- ICD device - The ICD device is implanted in the infraclavicular region as a pacemaker and consists of a capacitor apart from the battery, sensing amplifier, computer software and circuitry. The capacitor charges in a short period of a few seconds and delivers energy up to 40 Joules in the times of need. Hence, the size and weight of an ICD device is much larger than that of a pacemaker.
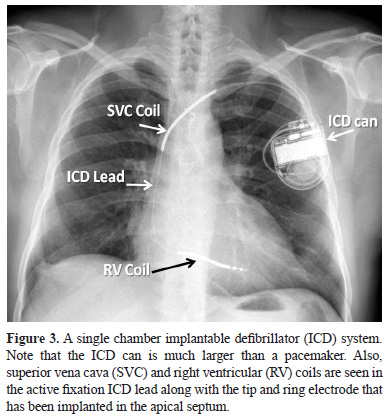
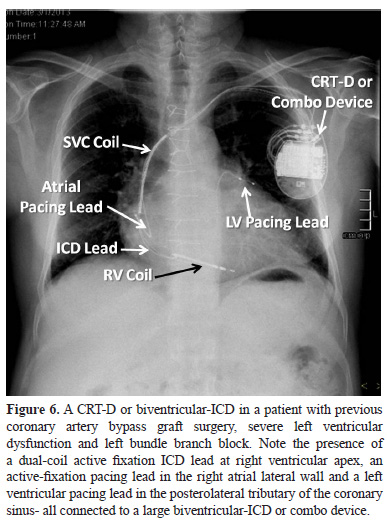
- ICD leads with shocking coils – The ICD lead is thicker than a pacemaker lead since apart from the tip and ring electrodes, it also has shocking coils (Figure 3 and 4). A single coil lead has a shocking coil in the right ventricle and a dual-coil lead has in addition another coil in the superior vena cava (Figure 3, 4 and 6). These coils along with the ICD device or can form the shocking vector during energy delivery. The ICD lead is implanted in a similar fashion as a pacemaker lead and again can have either passive or active fixation mechanisms.
The primary purpose of an ICD system is to detect, diagnose and treat a ventricular tachyarrhythmia – a ventricular tachycardia (VT) or a ventricular fibrillation (VF), the main determinant of which is the sensed ventricular rate. The ICD has tiered therapies – treats VT initially with pacing at a faster rate for a few beats (anti-tachycardia pacing or ATP) and if unsuccessful delivers a cardioversion shock. VF is directly treated by high energy defibrillation shock, though newer devices try to treat a VF episode by ATP while the device is charging. It should be understood that the ICD device differentiates a VT from VF primarily by its rate; hence a very fast clinical monomorphic VT in the VF zone will be diagnosed as VF by the device. The advantage of treating by an ATP is that it is faster, consumes less energy and most importantly is painless and harmless. In contrast, shock therapy is painful, and evokes anxiety and panic. Multiple shocks can even cause harm and increase mortality. Hence, the ICD needs to be programmed in such a way that shocks are minimized without compromising on the safety of the patient and without hindering timely treatment of VT and VF.
All ICDs also have bradycardia pacing capability.
Since most patients requiring ICD do not need pacing, single chamber ICD is used in most patients. The patients who also need pacing like those with sinus node dysfunction or AV block may be implanted with a dual –chamber ICD system. The dual-chamber ICD system has an atrial pacing lead in addition to an ICD lead and has the capability of dual-chamber pacing.
- ICD device - The ICD device is implanted in the infraclavicular region as a pacemaker and consists of a capacitor apart from the battery, sensing amplifier, computer software and circuitry. The capacitor charges in a short period of a few seconds and delivers energy up to 40 Joules in the times of need. Hence, the size and weight of an ICD device is much larger than that of a pacemaker.
- Cardiac Resynchronization Therapy (CRT) devices – An important fraction of patients with heart failure due to left ventricular systolic dysfunction have left bundle branch block (LBBB). LBBB results in inter- and intra-ventricular dyssynchrony that further impairs the cardiac output in these patients resulting in worsening of clinical outcome. CRT by pacing in both left and right ventricle in these patients results in narrowing of QRS complex, reduction in mitral regurgitation, improvement in left ventricular ejection fraction, reduction in heart failure symptoms and improvement in survival. Left ventricular pacing is achieved by implanting a lead in the tributary (usually posterolateral or lateral) of coronary sinus that stimulates the lateral or posterolateral part of left ventricle epicardially. Rarely, left ventricular pacing may not be possible via transvenous system due to technical reasons and then an epicardial lead is implanted in the left ventricle surgically. CRT devices are of two types:
- CRT-P system – Here there are atrial, right ventricular and left ventricular pacing leads connected to the pacemaker (Figure 5) and results in cardiac resynchronization. There is no capability of cardioversion or defibrillation in this system. Since it paces both right and left ventricles it is also commonly known as a biventricular pacemaker.

- CRT-D system – CRT-D system has right atrial and left ventricular pacing leads and a right ventricular ICD lead connected to a device that has capability of both resynchronization therapy as well as cardioversion-defibrillation (Figure 6). Since this device is a combination of biventricular pacemaker and an ICD, it is also known as biventricular-ICD or a Combo device.
- CRT-P system – Here there are atrial, right ventricular and left ventricular pacing leads connected to the pacemaker (Figure 5) and results in cardiac resynchronization. There is no capability of cardioversion or defibrillation in this system. Since it paces both right and left ventricles it is also commonly known as a biventricular pacemaker.
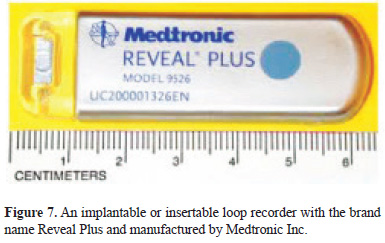
- Implantable Loop Recorder (ILR) – The cause of syncope remains undiagnosed in a large number of patients despite extensive non-invasive and invasive investigations. The mainstay of diagnosis remains the electrocardiographic rhythm analysis at the time of syncope that is impossible in an outpatient. ILR (Figure 7) are small devices that are implanted or inserted in subcutaneous region of the chest under local anesthesia and have the capability of storing single lead ECG like recording in circumstances of abnormal slow or fast rhythm or if activated by the patient. The patient is provided an instrument called activator that needs to pressed by the patient or attendants at the time of symptoms to activate the recording. The ILR records a loop of ECG for few seconds before and few seconds after activation. The stored electrograms can be retrieved in clinic using a programmer or remotely by wireless transmission through home monitoring systems. This provides the rhythm diagnosis at the time of syncope and my help in classifying the cause of syncope as non-arrhythmic, bradyarrhythmia (sinus pause or AV block) or a tachyarrhythmia (supraventricular tachycardia, VT or VF). ILR has been shown to have the maximum yield for the diagnosis of syncope among the commonly used investigative modalities. ILR can be explanted after a diagnosis of syncope is achieved or it reaches its end of life that is usually up to 3 years.
- Implantable Cardiovascular Monitor (ICM) - These are devices similar to pacemakers that not only provide rhythm diagnosis but also store other hemodynamic data like right ventricular or pulmonary artery pressure that can aid in the management of patients with chronic cardiac conditions such as heart failure. They are not in common clinical use at present but are likely to be utilized more and more in future as technological advances are made and their clinical utility established by large clinical trials.
Thus, it is clear that not all implantable electronic devices are pacemakers and it is of paramount importance for not only physicians & radiologists but also patients & their relatives to understand what kind of CIED a person has. A chest X-ray can not only help in identifying the type of device but also ascertain the device company by special radiological markers present on the device. Of course, it will help in detection of complications like lead dislodgement or fracture and device migration.
- Why Publish with JCPC?
- Instructions to the Authors
- Submit Manuscript
- Advertise with Us
- Journal Scientific Committee
- Editorial Policy
Print: ISSN: 2250-3528


