The Journal of Clinical and Preventive Cardiology has moved to a new website. You are currently visiting the old
website of the journal. To access the latest content, please visit www.jcpconline.org.
Case Report
Two Patients Presenting with QT Prolongation After Iohexol Contrast Medium
Volume 2, Jan 2013
Ali Çoner MD, Kaan Okyay MD, Bülent Özin MD, Ankara, Turkey
J Clin Prev Cardiol. 2013;2(1):48-52
IntroductionMore than 50 years ago, first selective coronary arteriography procedure was performed at the Cleveland Clinic. Since then, left heart catheterization has become a crucial part of diagnostic cardiology. Despite the advent of noninvasive imaging modalities, coronary arteriography remains the clinical gold standard for determining the presence of significant coronary artery disease. Left heart catheterization is an invasive procedure with serious risks. Major complications are uncommon (<1%) after coronary arteriography and include death, myocardial infarction (MI), contrast agent reactions, stroke and local vascular complications. According to Society for Coronary Angiography and Interventions (SCAI) Registry, arrhythmias are seen in 0.38% of the patients undergoing coronary arteriography, and the risk of arrhythmia is related to type and volume of contrast agent used (1). Herein, we present two patients with QT prolongation after coronary arteriography performed with iohexol, a non-ionic, low-osmolar contrast medium.
Case Reports
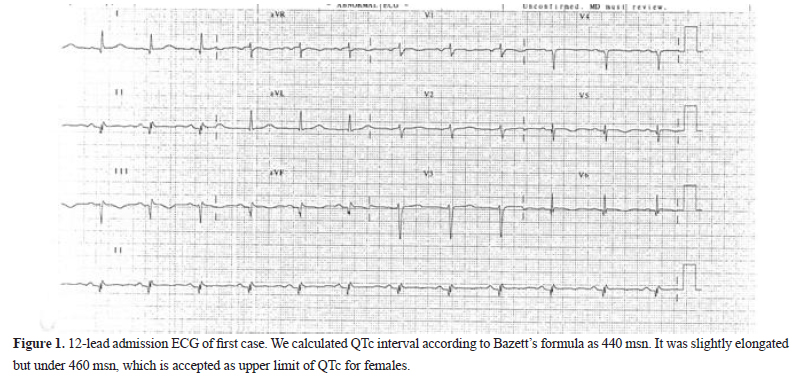
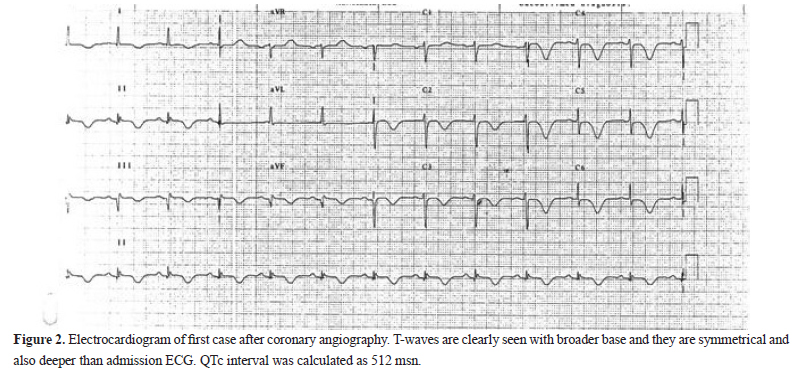
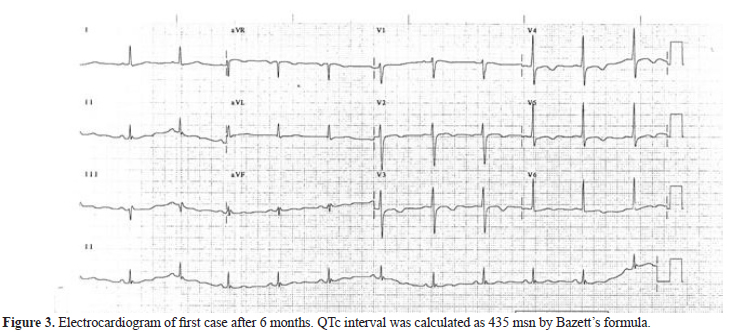
First patient was a 64-year-old female who was admitted to our cardiology outpatient clinic with complaints of palpitation and intermittent chest pain that lasted for one week. She had hyperlipidemia and hypertension in her past history. She had been using amlodipine 5 mg and atorvastatin 20 mg per day. Her physical examination revealed no specific finding. In her laboratory results, no specific finding was detected. Her estimated glomerular filtration rate was 50 mL/min/173m2 according to MDRD formula. In her admission electrocardiogram (ECG), there was a sinus rhythm with leftward axis. QTc interval was slightly prolonged and calculated as 440 msn (Figure 1). On her transthoracic echocardiography, apical hypokinesia was detected and heart valves were normally functioning. Coronary arteriography was performed using iohexol as the contrast agent. Coronary arteries were detected normal. After coronary arteriography, QTc interval was prolonged to 512 msn (Figure 2). The patient was hospitalized for 3 days for monitorization of this ECG finding. QTc interval was decreased gradually and calculated as 450 msn at discharge (Figure 3). She was seen at our outpatient clinic 6 months later, and QTc interval was calculated as 435 msn.
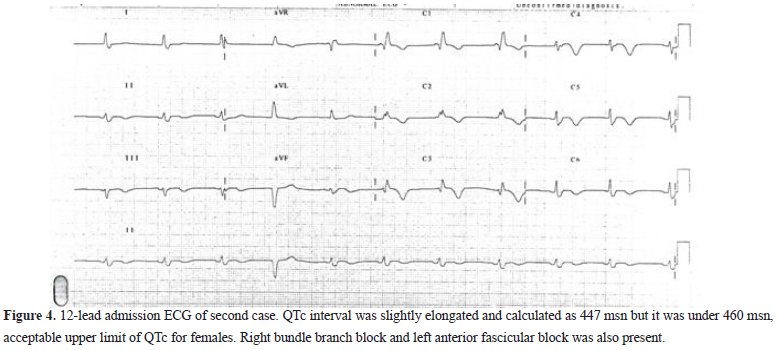
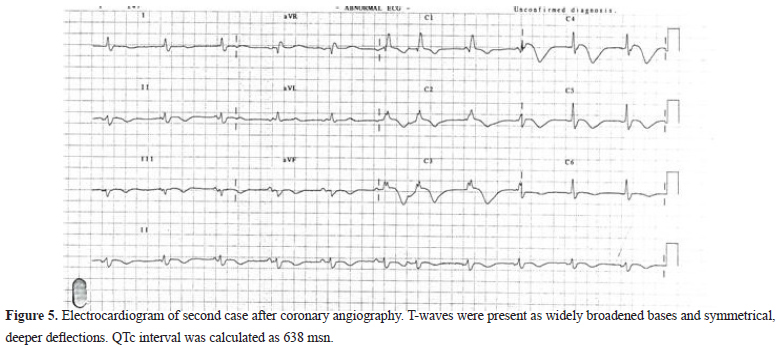
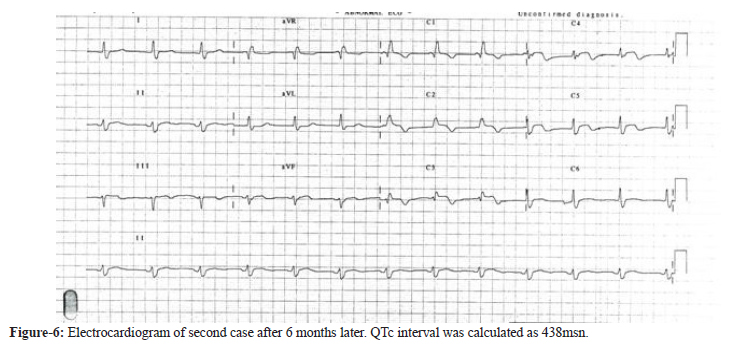
The second patient was an 82-year-old female who was admitted to our emergency department with anginal complaints. She had a history of hypertension and was using valsartan 160 mg per day. On physical examination, her blood pressure was slightly elevated (140/90 mmHg). In her laboratory results, troponin-I was slightly elevated and other results were detected normal. Her estimated glomerular filtration rate was 48 mL/min/ 173m2 according to MDRD formula. On admission ECG, right bundle branch block was found and QTc interval was calculated as 447 msn (Figure 4). On transthoracic echocardiography, normal systolic functions and normal heart valves were detected. Coronary arteriography was performed and 50% stenosis in distal left anterior descending artery was detected which was determined as noncritical. Coronary arteriography was performed with iohexol. After coronary arteriography, QTc was prolonged to 638 msn (Figure 5). After this ECG finding, the patient was monitorized for 4 days and QTc interval gradually decreased to 467 msn at discharge (Figure 6). One month later, at our outpatient clinic her QTc interval was calculated to be 438 msn. Both these patients were informed about their clinical situation and QTc prolongation. They were informed about drugs which have QTc prolongation effect including antibiotics. They were informed about hypovolemia and daily oral hydration amount. Blood electrolyte levels were monitored during outpatient controls.
QTc prolongations in these two patients following coronary arteriography were thought to be related to the exposure of iohexol contrast medium.
Discussion
Contrast agent selection is very important in the field of interventional cardiology due to steadily increased number of cardiovascular diagnostic procedures. All radiographic contrast agents contain iodine, which effectively absorbs X-rays in the energy range of the angiographic imaging system. Radiographic contrast agents currently used for coronary arteriography may also produce a number of adverse hemodynamic, electrophysiological, and renal effects. The key differences among contrast agents are their osmolality (low 600–900 mOsm/kg versus high 2000 mOsm/kg), whether they are ionic or non-ionic, and their cost.
Non-ionic agents do not ionize in solution and provide more iodine-containing particles per milliliter of contrast material compared to ionic agents. Their osmolality is substantially reduced (<850 mOsm) because these agents are obtained as single neutral molecules in solution and do not chelate calcium, leading to fewer side-effects. An ideal contrast agent for cardiovascular diagnostic and interventional procedures should have an osmolality isotonic to blood, a viscosity comparable to blood, and no influence on electrolyte balance (2). Iohexol is a non-ionic X-ray contrast medium of low osmolality, extensively used in cardiology and considered essentially free from side-effects of other contrast agents. Like other iodine-containing contrast media, it is eliminated from the body by excretion in urine. In patients with normal renal function, 97–99% of the intracoronary injected iohexol is excreted as unchanged through the kidneys within 24 hours. The maximum urinary concentration appears within approximately 1 hour after injection. The elimination half-life is 120–150 minutes in healthy subjects. Significant metabolism does not occur and protein binding is less than 2% (3).
The time course of the QT-prolongation effect of iohexol is not known. Our routine electrocardiography measurements were taken every 6 hours after cardiac catheterization. Assessment of these ECGs suggested that QT-prolongation time could be proportional to peak serum concentration of iohexol and peak effect is expected after 2 hours of injection given an unimpaired glomerular filtration (5).
Although basal QTc intervals were slightly elongated in both patients, they were under acceptable upper limit for females (4). In the first case, we detected mild apical hypokinesia but this finding did not add additional value to patient’s clinic according to us. Cardiac biomarkers were not elevated in serial followups and patient’s systolic functions remained same in the control echocardiography. In the second case, cardiac troponin-I was found slightly elevated but in serial followups, we did not detect any additional increase in troponin-I and also in creatinine kinase-MB bands. Also we did not detect any segmentary or global left ventricular systolic dysfunction in admission and control echocardiographies. We did not think other possible diagnosis like myocarditis in these two patients. QTc elongations were closely related with the iohexol administration.
Although iohexol is used commonly in interventional cardiology, there are limited data about effects of iohexol on QTc interval. In one study, in susceptible patients for QTc prolongation like patients taking amiodarone, QTc interval was found more prolonged than control group even with low-osmolar iohexol contrast medium (5). We know that QTc interval tends to be more prolonged normally in other susceptible conditions like elderly female population (4).
Our findings in these two patients are important for outpatient performed coronary angiographies, where the patients cannot have facilities for an adequate monitoring after application of contrast medium. In all patients, medications related to QT prolongation must be used cautiously, even iohexol which is known as reliable and having less side-effects. Especially in patients, like elderly females, susceptible to QTc prolongation contrast medium must be used judiciously. Low-osmolar contrast medium even like iohexol may cause QTc prolongation in these susceptible cases. Additionally, in these cases, screening of the serum electrolytes, especially avoiding from hypovolemia, hypokalemia and hypomagnesemia are the essential clinical aspects. In many cases, careful followup for potential risks and close monitoring of the patients are sufficient when the QTc prolongation is observed.
References
1. Popma JJ. Coronary arteriography. In: Braunwald E (ed). Heart Disease. Philadelphia, PA: Elsevier Saunders; 2012:406–40.
2. Altun A, Ozbay G. Effects of Ionic versus non-ionic contrast agents on dispersion of ventricular repolarization. Türk Kardiyol Dern Arş. 1998;26:362–7.
3. Bourin M, Jolliet P, Ballereau F. An overview of the clinical pharmacokinetics of X-ray contrast media. Clin Pharmacokinet. 1997;32:180–93.
4. Wagner GS, Lim TH. Interpretation of the normal electrocardiogram. In: Wagner GS (ed). Marriott’s Practical Electrocardiography. Philadelphia, PA: Lippincott Williams & Wilkins; 2008:43–70.
5. Goernig M, Kirmeier T, Krack A, Hartog C, Figulla H, Leder U. Iohexol contrast medium induces qt prolongation in amiodarone patients. Br J Clin Pharmacol. 2004;58:96–8.
- Why Publish with JCPC?
- Instructions to the Authors
- Submit Manuscript
- Advertise with Us
- Journal Scientific Committee
- Editorial Policy
Print: ISSN: 2250-3528


