The Journal of Clinical and Preventive Cardiology has moved to a new website. You are currently visiting the old
website of the journal. To access the latest content, please visit www.jcpconline.org.
Review Article
Prevention and Impact of Childhood Obesity in India
Volume 3, Jan 2014
Anoop Misra, MD, Swati Bhardwaj, PhD, New Delhi, India
J Clin Prev Cardiol. 2014;3(1):5-11
IntroductionObesity has reached epidemic proportions globally and its prevalence has doubled in the last two decades (1). Over the last 5 years, most developing countries have reported prevalence rates of obesity (inclusive of overweight) > 15% in children and adolescents aged 5–19 year (2–4). Childhood obesity is increasing at an alarming pace in India, giving rise to adult diseases in youth, like high blood pressure, type 2 diabetes mellitus (T2DM), heart disease and osteoporosis.
Defining Childhood Obesity: Diagnostic Criteria
The criteria for assessing childhood obesity have been the subject of debate and research. The following criteria for age- and gender-specific body mass index (BMI)ABSTRACTcutoffs have been applied by different groups to diagnose childhood obesity.
- IOTF (International Obesity Task Force) cutoffs. Cole et al. (2000) developed international cutoffs for children aged 2–18 year from varied ethnicities (Brazil, United Kingdom, Hong Kong, The Netherlands, Singapore, and USA, including 97,876 males and 94,851 females from birth to 25 year of age) (5). Percentile curves that corresponded to the BMI cutoff points of 25 and 30 kg/m2 at the age of 18 year were used to define overweight and obesity, respectively. These cutoffs are meant to provide more internationally comparable prevalence rates of overweight and obesity in children.
- CDC (Centers for Disease Control and Prevention) BMI percentiles (6). BMI percentile curves were developed in a nationally representative population of North American children, aged 2–20 year (overweight 85–94th percentile; obese >95th percentile).
- WHO (World Health Organization) growth reference curves (7). These curves were developed in 2007 for children and adolescents aged 5–19 yr to align with the recommended adult cutoffs for overweight and obesity at 19 yr (overweight: > +1 SD; obese: > +2 SD).
- WHO growth standards (1995) (8,9). These standards were based on data collected in USA as recommended by a 1995 WHO Expert Committee. Weight-for-height Z score >1 and >2 were used to define overweight and obesity, respectively, in preschool children (< 5 year).
- New WHO growth standards in preschool children (2006) (10). These standards were developed using data collected in the WHO Multicenter Growth Reference Study (1997–2003) from approximately 8500 children from widely different ethnic backgrounds and cultural settings (Brazil, Ghana, India, Norway, Oman, and the USA). The new growth curves are expected to provide a single international standard for best physiological growth for all children from birth to 5 years of age and to establish the breastfed infant as the normative model for growth and development. Overweight is defined as BMI for-age Z score of 1 or higher and obesity as BMI-for-age Z score of 2 or higher.
Prevalence
There is a wide variation in the prevalence data for childhood obesity globally. In 2010, 43 million children (35 million in developing countries) were estimated to be overweight and 92 million were at risk of being overweight (11). The worldwide prevalence of childhood overweight and obesity increased from 4.2% (95% CI: 3.2%, 5.2%) in 1990 to 6.7% (95% CI: 5.6%, 7.7%) in 2010. Data from many developing countries show an increase in prevalence of obesity in children and adolescents (12–17).
To date, very few nationally representative reports are available on the prevalence of obesity among Asian Indian children and adolescents living in India. The prevalence of overweight/obesity in urban post-pubertal children in Delhi showed an increase from 16% in 2002 to about 24% in 2006 (15). A high prevalence was seen in the private schools (catering to children from upper socioeconomic stratum) 29% versus 11% in government schools (catering to lower socioeconomic stratum) (12, 16, 17). A recent multicentric cross-sectional study in 38,296 children from five urban cities located in different geographical regions of India showed that the prevalence of overweight and obesity in 8- to 18-year-old children was 14.4% and 2.8% by IOTF cutoffs, 14.5% and 4.8% by CDC cutoffs, and 18.5% and 5.3% by WHO cutoffs, respectively (17). Also, the overall prevalence of abdominal obesity (defined according to the International Diabetes Federation consensus statement for at-risk children and adolescents) (18) in these children was 4.5%.
Determinants
The increasing trend of overweight prevalence is documented among children/adolescents (5–19 year) because of the following sociocultural factors:
- Unhealthy nutrition. Comparatively low cost of energy-dense foods, improved purchasing power, television advertisements targeting children and junk foods being sold in the school cafeterias are shifting the children’s dietary habits from healthy foods to fried fatty and processed foods.
- Working status of parents. Parents these days are both working and have a hectic lifestyle. They are often overworked and it is easy to let children order “fast foods” and hardly have any time to oversee balanced nutrition for children.
- Lack of physical activity. Shift from outdoor play to indoor entertainment; television viewing, Internet and computer games has attributed to increased childhood obesity. Children no longer want to ride a cycle and parents feel it is safer to ride a car than a cycle in a chaotic city.
- Academics. Increasing burden of academic competitiveness among students have led to decreased participation in sports and any other form of physical activity. This is particularly true for girls who are sedentary from school years. Many of the studies from India show that females have more obesity and the metabolic syndrome as compared to males.
- Increased Socioeconomic status. Increased purchasing power in the form of daily allowance (pocket money) to purchase foods/snacks available in school cafeteria or nearby fast food joints could be a major reason for this.
- Wrong parental approach. Parents in India and other developing countries usually have a general misconception that an obese child is a healthy child. And that if the child is fat, “baby fat” will go away with time. In an effort to keep child “healthy,” he/she is fed in excess. Many of these children remain obese for the lifetime.
- Technology. Most importantly with the advancement in technology, especially in the field of entertainment more time is spent in front of television, computers and video games at the expense of sports and physical activity, making it a sedentary lifestyle for the children.
Impact of Childhood Obesity
In the last one decade, childhood obesity has been increasingly implicated as a primary childhood health
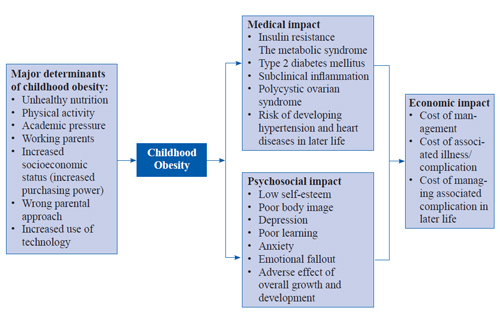
problem. Obesity is associated with several comorbid conditions: dyslipidemia, hypertension, hyperglycemia, non-alcoholic fatty liver disease (NAFLD) and a conglomeration of conditions known as the metabolic syndrome (19). As a result of childhood obesity, health problems such as hypertension, T2DM and hypercholesterolemia that were once confined to adults are now being diagnosed in children. Figure 1 gives an overview of childhood obesity (determinants and impact).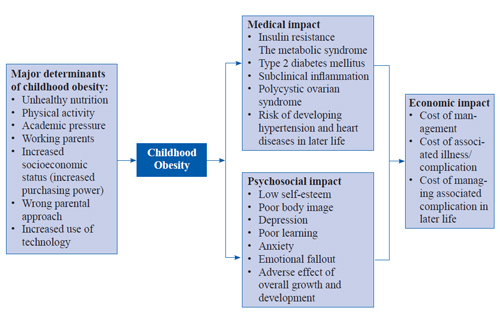
Medical Impact
Insulin resistance and the metabolic syndrome
Association of multiple factors like central obesity, dyslipidemia (hypertriglyceridemia and low levels of high-density lipoprotein-cholesterol), hypertension and impaired glucose tolerance (IGT) characterizes the metabolic syndrome. About one-third of overweight or obese urban Asian Indian children have insulin resistance (13). Interestingly, higher level of hyperinsulinemia and related metabolic derangements has been recorded in Asian Indian neonates and children as compared to white Caucasian neonates (20). Similar comparative data are available for young children indicating early occurrence of insulin resistance in Asian Indians (14). Data pertaining to the metabolic syndrome in children and adolescents are limited due to lack of a well-established definition for the metabolic syndrome in children. Importantly, the pattern of weight gain, particularly rapid weight gain after the age of 2 year, has been shown to be significantly associated with a higher prevalence of the metabolic syndrome in young (26–32 year) Asian Indians (21). Recently, in a factorial analysis, obesity/insulin factor (BMI, waist circumference [WC], triceps skinfolds, subscapular skinfolds, and fasting insulin) was shown to be independently associated with a high cumulative risk of the metabolic syndrome in urban Asian Indian adolescents (22). Insulin resistance has been reported to be present as early as 8 year of age in Asian Indian children (23), with an overall prevalence of fasting hyperinsulinemia in 29.0% and 63.9% normal weight and overweight adolescents (BMI > 23 kg/m2), respectively (24).
Type 2 diabetes mellitus
Obesity, especially abdominal obesity, is among the strongest risk factors for T2DM. Globally, T2DM is being reported at an early age, primarily contributed by obesity and the metabolic syndrome in early childhood.We have reported that generalized obesity and abdominal obesity were significantly higher in children and adolescents with T2DM in North India (24). Important independent risk factors for development of T2DM in Asian Indian adolescents and young adults were hypertriglyceridemia, high waist-to-hip ratio and family history of diabetes (25).
Subclinical inflammation
Obesity contributes to the development of vascular inflammation which raises markers of inflammation. Subclinical inflammation, typified by markers such as high-sensitivity C-reactive protein (hs-CRP), is associated with atherosclerosis and has been shown to predict T2DM and CAD (26). Generalized and abdominal adiposity has been shown to be independently associated with increased levels of hs-CRP in Asian Indian adolescents and young adults (aged 14–25 year) (25). In this study, high hs-CRP levels were seen in 13% of Asian Indian adolescents overall, in approximately 22% of overweight (BMI 85th percentile) and in approximately 25% of those with excess body fat (percent body fat >85th percentile). CRP levels show an association with percentage of body fat, waist-to-hip ratio, WC and triceps skinfold thickness in Asian Indian children. Interestingly, excess dietary intake of saturated fat was a strong correlate of high CRP levels in Asian Indian adolescents (27).
Polycystic ovarian syndrome (PCOS)
Obese adolescent girls are more likely to suffer from PCOS, a syndrome of variable combinations of menstrual irregularity, hirsutism or acne, with obesity and insulin resistance. Higher prevalence of PCOS was reported in South Asian women than white Caucasians in a recent study (28). South Asians present and seek treatment of PCOS at a younger age than white Caucasians, have more severe symptoms, and higher fasting insulin concentrations and lower insulin sensitivity than white Caucasians. The prevalence and course of PCOS in developing countries has not been adequately investigated.
With the rapid rise in childhood obesity, there has also been an increase in the prevalence, recognition and severity of pediatric NAFLD (29). Although prevalence of NAFLD is high in some developing countries (30), relevant data in children from developing countries are not available, and this issue needs to be researched further.
Psychosocial impact of childhood obesity
Overweight and obese adolescents tend to have poor body image and low self-esteem. Social isolation and stress could interfere with their learning and lead to depression, anxiety and emotional fallout. These negative factors work against the child with a weight problem and thus hamper his/her overall growth and development (31). In this context, no other data are available from developing countries like India.
Economic impact
Apart from medical and psychosocial impact, childhood obesity also causes huge economic impact on the individual families, healthcare sector as well as the country. It would be difficult to estimate the total financial burden caused by childhood obesity as this computation would not only include the cost involved in managing the condition but also the complete analysis of cost of illness caused as a complication of childhood obesity and also its medical impact in later life, if left unmanaged. There is hardly any data in India to quantify the economic impact of childhood obesity; however, in the developed countries there have been attempts to estimate the cost factor associated with childhood obesity and its management, based on the impact of obesity on healthcare utilization and expenditures during childhood. Hampl et al. (2007) found that children in a large pediatric integrated delivery system diagnosed with obesity during a healthy-child visit had US$172 higher annual healthcare expenditures than children with a normal BMI (32). An analysis of the 2001–2003 Medical Expenditure Panel Survey (MEPS) identified that overweight children, defined by the American Medical Association Expert Committee and other national associations as children with a BMI in the 85–94th percentile for age and sex, had annual total healthcare expenditures US$180 higher than children with a normal BMI, while obese children, or children with a BMI in the 95th percentile or greater for age and sex, had US$220 higher expenditures on average (33, 34).
Prevention
For prevention of obesity especially during childhood emphasis should be laid on a healthy and active lifestyle and creating a nurturing environment that helps the youth recognize their own worth and respect cultural food ways. It is recognized that obesity, eating disorders, hazardous weight loss, nutrient deficiencies and size discrimination are all interrelated and need to be addressed in a comprehensive manner, thus requiring a multilevel approach. Some of the recommendations that can help in preventing and reducing childhood obesity in developing countries are shown in Table 1.
Table 1.
Community-based interventions should aim at providing a conducive environment for children to follow a healthy lifestyle, promote healthy food alternatives and bring awareness and need about an increase in physical activity.
Community intervention programs for childhood obesity in India
Community-based interventions are aimed at generating awareness and providing a conducive environment for children to follow a healthy lifestyle (balanced diet and increased physical activity) and promote healthy food alternatives. In India, we have initiated comprehensive programs aiming at childhood obesity, namely “CHETNA” (Children Health Education through Nutrition and Health Awareness program, Hindi for “The Awareness”), which was carried out in New Delhi and “MARG” (Medical Education for Children/Adolescents for Realistic Prevention of Obesity and Diabetes and for Healthy Ageing, Hindi for “The Path”), carried out in 15 cities of North India covering nearly 700,000 children. Under these programs, children are given nutritional and physical activity education with the help of lectures, leaflets, debates and skits. These comprehensive programs initiated on a large scale for the first time in South Asia aimed to impart education regarding healthy lifestyle not only to children, but also to teachers and parents. The MARG program is the first large-scale community intervention project in South Asia, which focuses 100% on primary prevention of not only diabetes, but on non-communicable diseases in general.
Conclusion
Childhood obesity is associated with a number of health problems such as hypertension, T2DM and hypercholesterolemia, IGT, which were once confined to adults. It is also associated with significant other morbidities including gallstone, dyslipidemia, obstructive sleep apnea syndrome, early puberty or menarche, eating disorders, skin infections, orthopedic disorders, asthma and other respiratory disorders. Apart from medically impacting the individual, childhood obesity also adversely impacts the psychosocial development of the child as well as the financial economy of the individual household as well as the country. Thus, for prevention of obesity, emphasis should be laid on a healthy and active lifestyle and creating a nurturing environment that helps the youth recognize their own worth and respect cultural food ways. It is recognized that obesity, eating disorders, hazardous weight loss, nutrient deficiencies and size discrimination are all interrelated and need to be addressed in a comprehensive manner. Community-based interventions should aim at providing a conducive environment for children to follow a healthy lifestyle, promote healthy food alternatives, and generate awareness about an increase in physical activity.
Conflict of Interest
Authors do not have any conflicts of interest.
Acknowledgement
We acknowledge the support and cooperation of National Diabetes, Obesity, and Cholesterol Disorders Foundation (N-DOC), New Delhi, Diabetes Foundation (India), and World Diabetes Foundation, Denmark, in various research initiatives in childhood obesity undertaken by our group.
References
- Gupta N, Shah P, Nayyar S, Misra A. Childhood obesity and the metabolic syndrome in developing countries. Indian J Pediatr. 2013;80:S28–37.
- de Assis MA, Rolland-Cachera MF, Grosseman S, de Vasconcelos FA, Luna ME, Calvo MC, Barros MV, Pires MM, Bellisle F. Obesity, overweight and thinness in schoolchildren of the city of Florianopolis, Southern Brazil. Eur J Clin Nutr. 2005;59:1015–21.
- Moraes SA BRJ, Mondini L, Freitas IC. Prevalence of overweight and obesity, and associated factors in school children from urban area in Chilpancingo, Guerrero, Mexico, 2004. Cad Saude Publica. 2006;22:1289–301.
- Pituelli Suarez N, Corbera Prin M, Lioi Luciani S, Turco Pilotto M, D’Arrigo Dri M, Rosillo Politti I. [Prevalence of risk factors: obesity and lipid profile]. An Pediatr (Barc). 2008;68:257–63.
- Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320:1240–3.
- Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, Mei Z, Curtin LR, Roche AF, Johnson CL. CDC growth charts: United States. Adv Data. 2000;(314):1–27.
- Butte NF, Garza C, de Onis M. Evaluation of the feasibility of international growth standards for school-aged children and adolescents. J Nutr. 2007;137:153–7.
- World Health Organization. 1995. Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. Tech Rep Ser 854. Geneva: World Health Organization.
- WHO Multicentre Growth Reference Study Group 2006 WHO child growth standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: methods and development. Geneva: World Health Organization.
- World Health Organization WHO child growth standard 2006. http://www.who.int/childgrowth. Date accessed, November 1, 2013.
- De Onis M, Blössner M, Borghi E. Global prevalence and trends of overweight and obesity among preschool children. Am J Clin Nutr. 2010;92:1257–64.
- Bhardwaj S, Misra A, Khurana L, Gulati S, Shah P, Vikram NK. Childhood obesity in Asian Indians: a burgeoning cause of insulin resistancediabetes and sub-clinical inflammation. Asia Pac J Clin Nutr. 2008;17:172–5.
- A, Dwivedi M, Sharma R, Luthra K, Guleria R, Talwar KK. High prevalence of insulin resistance in post-pubertal Asian Indian children is associated with adverse truncal body fat patterning, abdominal adiposity and excess body fat. Int J Obes Relat Metab Disord. 2004;28:1217–26.
- Misra A, Khurana L, Vikram NK, Goel A, Wasir JS. Metabolic syndrome in children: current issues and South Asian perspective. Nutrition. 2007;23:895–910.
- Singhal N, Misra A, Shah P, Rastogi K, Vikram NK. Secular trends in obesity, regional adiposity and metabolic parameters among Asian Indian adolescents in North India: A comparative data analysis of two selective samples 5 years apart (2003, 2008). Ann Nutr Metab. 2010;56:176–81.
- Raj M, Sundaram KR, Paul M, Deepa AS, Kumar RK. Obesity in Indian children: time trends and relationship with hypertension. Natl Med J India. 2007;20:288–93.
- Misra A, Shah P, Goel K, Hazra DK, Gupta R, Seth P, Tallikoti P, Mohan I, Bhargava R, Bajaj S, Madan J, Gulati S, Bhardwaj S, Sharma R, Gupta N, Pandey RM. The high burden of obesity and abdominal obesity in urban Indian schoolchildren: a multicentric study of 38,296 children. Ann Nutr Metab. 2011;58:203–11.
- Zimmet P, Alberti KG, Kaufman F, Tajima N, Silink M, Arslanian S, Wong G, Bennett P, Shaw J, Caprio S; IDF Consensus Group. The metabolic syndrome in children and adolescents - an IDF consensus report. Pediatr Diabetes. 2007;8:299–306.
- Nigam P, Bhatt SP, Misra A, Vaidya M, Dasgupta J, Chadha DS. Non-alcoholic fatty liver disease is closely associated with sub-clinical inflammation: a case-control study on Asian Indians in North India. PLoS One. 2013;8:e49286.
- Yajnik CS, Lubree HG, Rege SS, Naik SS, Deshpande JA, Deshpande SS, Joglekar CV, Yudkin JS. Adiposity and hyperinsulinemia in Indians are present at birth. J Clin Endocrinol Metab. 2002;87:5575–80.
- Fall CH, Sachdev HS, Osmond C, Lakshmy R, Biswas SD, Prabhakaran D, Tandon N, Ramji S, Reddy KS, Barker DJ, Bhargava SK; New Delhi Birth Cohort. Adult metabolic syndrome and impaired glucose tolerance are associated with different patterns of BMI gain during infancy: Data from the New Delhi Birth Cohort. Diabetes Care. 2008;31:2349–56.
- Vikram NK, Pandey RM, Misra A, Goel K, Gupta N. Factor analysis of the metabolic syndrome components in urban Asian Indian adolescents. Asia Pac J Clin Nutr. 2009;18:293–300.
- Bavdekar A, Yajnik CS, Fall CH, Bapat S, Pandit AN, Deshpande V, Bhave S, Kellingray SD, Joglekar C. Insulin resistance syndrome in 8-year-old Indian children: small at birth, big at 8 years, or both? Diabetes. 1999;48:2422–9.
- Vikram NK, Misra A, Pandey RM, Luthra K, Wasir JS, Dhingra V. Heterogeneous phenotypes of insulin resistance and its implications for defining metabolic syndrome in Asian Indian adolescents. Atherosclerosis. 2006;186:193–9.
- Vikram NK, Misra A, Dwivedi M, Sharma R, Pandey RM, Luthra K, Chatterjee A, Dhingra V, Jailkhani BL, Talwar KK, Guleria R. Correlations of C-reactive protein levels with anthropometric profile, percentage of body fat and lipids in healthy adolescents and young adults in urban North India. Atherosclerosis. 2003;168:305–13.
- Biasillo G, De Maria GL, Leo M, Stefanelli A, Biasucci LM. [Relation of C-reactive protein and coronary heart disease. Current knowledges]. Recenti Prog Med. 2009;100:279–85.
- Arya S, Isharwal S, Misra A, Pandey RM, Rastogi K, Vikram NK, Dhingra V, Chatterjee A, Sharma R, Luthra K. Creactive protein and dietary nutrients in urban Asian Indian adolescents and young adults.Nutrition. 2006;22:865–71.
- Wijeyaratne CN, Balen AH, Barth JH, Belchetz PE. Clinical manifestations and insulin resistance (IR) in polycystic ovary syndrome (PCOS) among South Asians and Caucasians: is there a difference? Clin Endocrinol (Oxf). 2002;57:343–50.
- Dunn W, Schwimmer JB. The obesity epidemic and nonalcoholic fatty liver disease in children. Curr Gastroenterol Rep. 2008;10:67–72.
- Bajaj S, Nigam P, Luthra A, Pandey RM, Kondal D, Bhatt SP, Wasir JS, Misra A. A case-control study on insulin resistance, metabolic co-variates & prediction score in non-alcoholic fatty liver disease. Indian J Med Res. 2009;129:285–92.
- Lee YS. Consequences of childhood obesity. Ann Acad Med Singapore. 2009;38:75–7.
- Hampl SE, Carroll CA, Simon SD, Sharma V. Resource utilization and expenditures for overweight and obese children. Arch Pediatr Adolesc Med. 2007;161:11–4.
- Expert Committee Recommendations on the Assessment, Prevention, and Treatment of Child and Adolescent Overweight and Obesity www.ama-assn.org/ama1/pub/upload/mm/433/ped_obesity_recs.pdf assessed 1st December, 2013.
- Finkelstein EA, Trogdon JG. Public health interventions for addressing childhood overweight: analysis of the business case. Am J Public Health. 2008;98:411–5.
- Gupta N, Goel K, Shah P, Misra A. Childhood obesity in developing countries: epidemiology, determinants, and prevention. Endocr Rev. 2012;33:48–70.
- Why Publish with JCPC?
- Instructions to the Authors
- Submit Manuscript
- Advertise with Us
- Journal Scientific Committee
- Editorial Policy
Print: ISSN: 2250-3528



.jpg)