The Journal of Clinical and Preventive Cardiology has moved to a new website. You are currently visiting the old
website of the journal. To access the latest content, please visit www.jcpconline.org.
Student's Page
Paroxysmal Narrow QRS Tachycardia
Volume 1, Apr 2012
Dr. Kartikeya Bhargava; MD, DNB, Gurgaon, India
Volume 1, April 2012
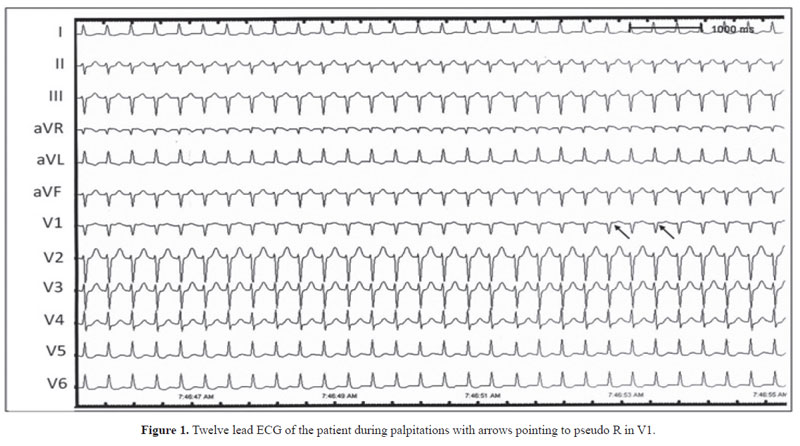
A 41-year-old gentleman presented with history of recurrent episodic palpitations of sudden onset. The baseline ECG showed left axis deviation of the QRS in the frontal plane with possible left anterior hemiblock and 2D echocardiography was normal (not shown). The ECG during one of the episodes is shown in Fig. 1. What is the ECG diagnosis?The ECG shows a narrow QRS regular tachycardia with heart rate of 200/min. The QRS morphology was identical to that during sinus rhythm. This is a classical example of paroxysmal supraventricular tachycardia (PSVT) – paroxysmal because it is episodic and occurs suddenly, supraventricular because it is narrow QRS with identical QRS morphology to that during sinus rhythm, and tachycardia since the heart rate is greater than 100/min. A supraventricular tachycardia is defined as any tachycardia that involves tissues above the His-bundle (supraventricular) as an essential part of the tachycardia circuit. Cardiac tissues below the His bundle including the ventricles may or may not be the part of the SVT circuit. Mostly, the PSVT is of narrow QRS (QRS duration < 120 ms) but at times can have wide QRS if there is preexisting bundle branch block or aberrant intraventricular conduction during tachycardia or if it involves antegrade conduction over an accessory atrioventricular connection.
In contrast, a ventricular tachycardia (VT) arises in the ventricular tissue and tissues above the Hisbundle bifurcation are not essential for the initiation or continuation of the tachycardia. Usually, VT has a wide QRS (QRS duration ≥ 120 ms) since there is sequential activation of the two ventricles but can very rarely have a narrow QRS if the VT arises in the interventricular septum very close to the normal His-Purkinje system.
PSVT is commonly due to the following mechanisms:
- Atrioventricular nodal reentrant tachycardia (AVNRT) – the tachycardia reentry circuit lies in the AV node and comprises of slow and fast AV nodal pathways. AVNRT is the most common (50%) cause of PSVT.
- Atrioventricular reciprocating tachycardia (AVRT) – the tachycardia is mediated by an atrioventricular accessory connection that conducts retrogradely during the narrow QRS SVT. The antegrade limb of the reentry circuit is via the normal AV node-His- Purkinje system. AVRT comprises approximately40% of all PSVTs.
- Atrial Tachycardia – the tachycardia arises at a focus in the left or the right atrium and thus is AV node independent. It is an uncommon cause of PSVT, accounting for less than 10% of cases.
AVNRT is of two varieties: (a) typical wherein the slow AV nodal pathway is the antegrade limb of the circuit and fast AV nodal pathway the retrograde limb and (b) atypical in which the circuit is reverse. In typical AVNRT, the most common cause of PSVT, the retrograde atrial activation occurs over the fast AV nodal pathway and is very rapid, almost simultaneous with the activation of the ventricles. Thus, the P-waves are either buried in the QRS (not seen) or occur just at the end of the QRS. In the latter instance, they produce a small deflection at the end of QRS resulting in pseudo R in V1 (see Fig. 1 arrows) or pseudo S in leads II, III, and aVf. Thus, V1 showing pseudo R-wave during a narrow QRS PSVT that is absent during sinus rhythm is almost diagnostic of AVNRT.
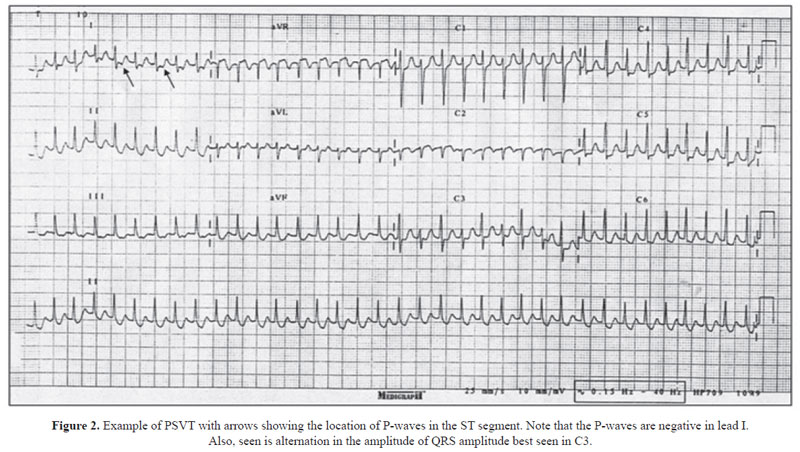
In contrast, the reentry circuit in AVRT is large with activation of the atria occurring after the ventricles via retrograde conduction in the accessory pathway that connects the atrium with the ventricle. Thus, the P-wave in an AVRT is seen in the ST segment quite later than the QRS (Fig. 2). Also, the morphology of the P-wave helps in determining the location of the atrial end of the accessory pathway. In the example shown in Fig. 2, the P-waves are negative in lead I indicating that the atrial activation is occurring from left to right (as opposed to right to left atrial activation seen during sinus rhythm when the P-wave is positive in lead I) and suggesting that the tachycardia is an AVRT mediated by a left lateral accessory pathway. Often, the ST depression produced by negative P-waves during an AVRT is misinterpreted as myocardial ischemia.
The exact mechanism of the PSVT whether AVNRT or AVRT is not of much importance for the clinician for the acute management since both are AV node dependent. Any maneuver or drug that blocks or delays conduction in the AV node even transiently will break the reentrant circuit and terminate the arrhythmia whether it is AVNRT or AVRT. The maneuvers include carotid sinus massage that by stimulating the carotid baroreceptors causes AV nodal slowing and terminates the PSVT or vagal maneuvers like pressing the eye balls, splashing cold water over the face, or valsalva maneuver. If these do not work, drug of choice is intravenous adenosine in a dose of 6–12 mg, given as a rapid bolus through a central or a large peripheral vein followed immediately by rapid saline flush. This drug causes transient AV nodal block and terminates the arrhythmia. It has a very short halflife (less than 10 seconds) and hence needs to be injected very rapidly. Flushing and a sense of discomfort are common but very short lasting side-effects. Adenosine is almost always successful in terminating PSVT due to AVNRT or AVRT, if administered properly. If it is not available or is ineffective, intravenous beta-blockers like metoprolol or calcium channel blockers like diltiazem or verapamil can be used. The side-effects of these medications include bradycardia, hypotension, and exacerbation of asthma (with beta- blockers).
The long-term management aims at prevention of recurrences and is done by either using oral beta-blockers or calcium channel blockers or more definitively by radiofrequency (RF) ablation. RF ablation is an invasive procedure wherein the tachycardia is induced in the electrophysiology lab, its mechanism determined, and the target tissue (e.g., the slow pathway in AVNRT or accessory pathway in AVRT) is ablated using RF energy. It is a highly successful procedure (more than 95%) with very low risk of complications (less than 2%) in expert hands and achieves a total cure in patients with PSVT.
Recognition of the mechanism of PSVT by ECG can help the cardiac electrophysiologist for planning RF ablation.
- Why Publish with JCPC?
- Instructions to the Authors
- Submit Manuscript
- Advertise with Us
- Journal Scientific Committee
- Editorial Policy
Print: ISSN: 2250-3528


