The Journal of Clinical and Preventive Cardiology has moved to a new website. You are currently visiting the old
website of the journal. To access the latest content, please visit www.jcpconline.org.
Review Article
OPCAB- Is It the “Best Technique” for Coronary Revascularization?
Volume 4, Oct 2015
Dheeraj Arora, DNB, PDCC, Yatin Mehta, MD, MNAMS, FRCA, FAMS, FIACTA Naresh Trehan, MD, Gurgaon, India
2015;4(4):89-97
IntroductionCoronary artery disease (CAD) is one of the commonest cardiovascular disorders. The management of CAD is both pharmacological or interventional that includes percutaneous catheter intervention (PCI) or coronary artery bypass grafting (CABG). The indication of the intervention depends upon the severity i.e. number and quality of the diseased vessels and associated co-morbidities. Severe CAD such as three-vessel disease (TVD) and left main disease (LMD) are considered as indications of CABG.
Traditionally CABG is performed with the use of cardiopulmonary bypass (CPB). In 1967, first successful CABG with saphenous vein was performed using CPB (1). Gradually the number of CABG’s increased over the years in United States of America (USA) majority of them being performed using CPB (2). Major disadvantages of conventional CABG (CCAB) are neuropsychiatric dysfunction, acute renal failure (ARF), coagulopathy, platelet dysfunction, systemic inflammatory response syndrome (SIRS), post-pump syndrome, postoperative pain, expense and longer convalescence (3).
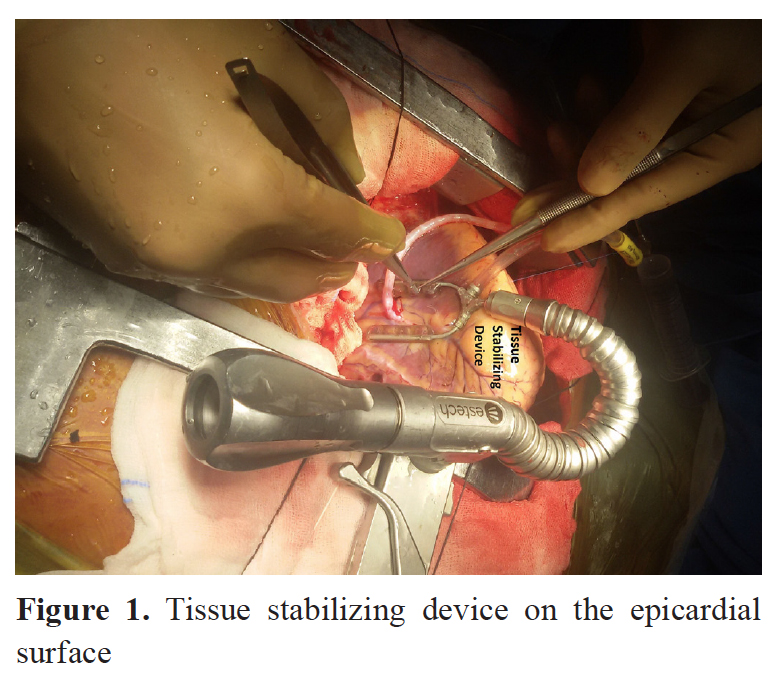
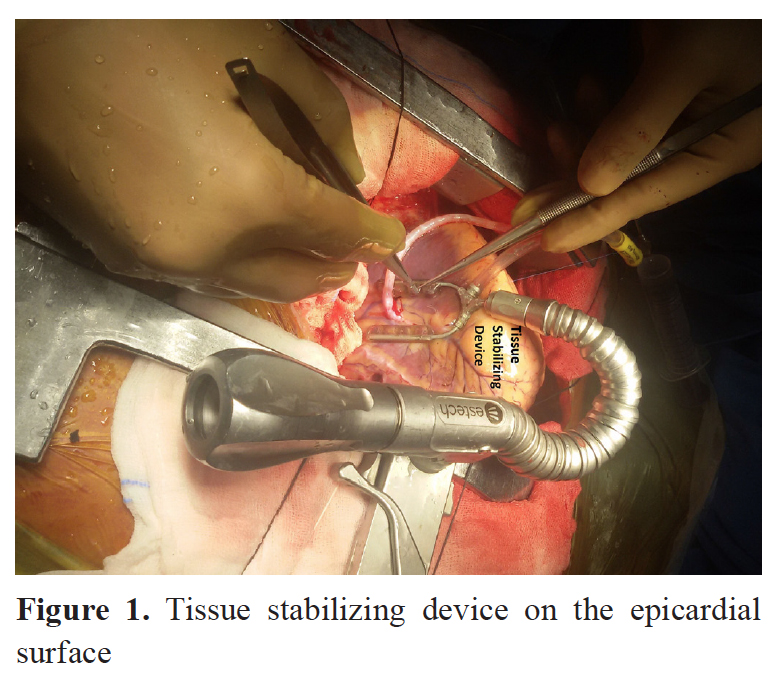
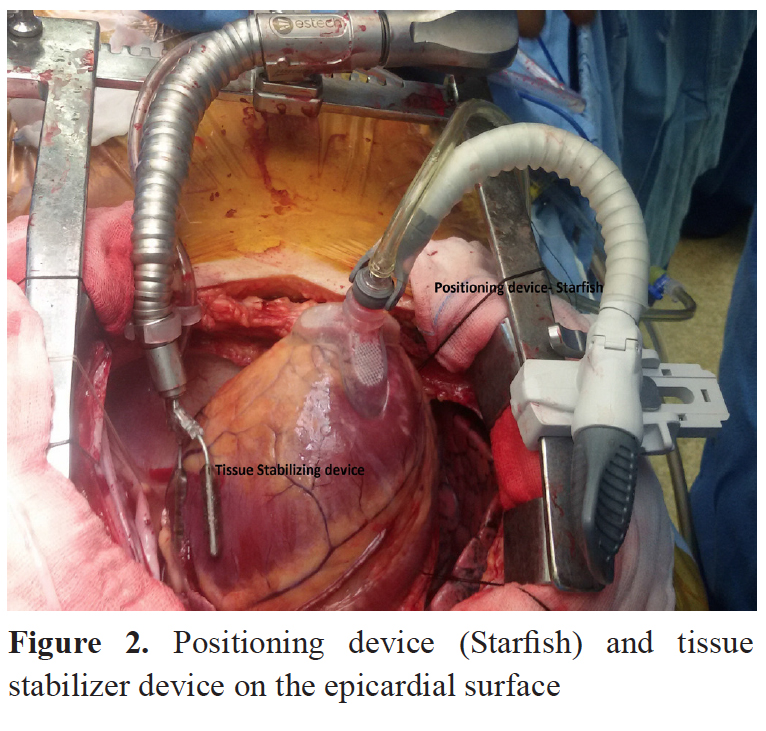
Off pump CABG (OPCAB) is performed without the use of CPB i.e. on the beating heart, with the help of specially designed epicardial wall stabilizers. History of OPCAB dates back to pre CPB era in 1950s when CPB itself was in incipient stage. But with the availability and wide acceptability of CPB, OPCAB went out of repute. Kolessov performed OPCAB in 1964 through a left thoracotomy incision on a beating heart, successfully grafted the internal mammary artery to branches of the left coronary artery (4). 1980s witnessed OPCAB with use of drugs like esmolol for reduction of heart rate which is desired by the surgeons during OPCAB. In 1990s the development of techniques like pericardial retraction suture, slings along with stabilization devices led to the resurgence of OPCAB as an acceptable alternative technique to perform CABG. Also in 1990s minimally invasive technique, suction stabilization and multivessel suction stabilization devices (Figure 1,2) were used for OPCAB (5-7).
Indications & Contraindications
Major advantage of OPCAB is to avoid CPB related complications particularly in patients whom CPB may increase the mortality or morbidity like recent or acute myocardial infarction, left ventricular (LV) dysfunction, renal failure, previous stroke, chronic obstructive airway disease (COAD), age more than 70 years, atheromatous aorta and unstable angina (8).Major contraindications for OPCAB are inexperienced surgeon, intracavitary thrombi like left ventricular clot, intramyocardial vessels, malignant arrhythmias, combined valve or ventricular repair, very small (<1mm) or calcified coronary arteries, poor vascular conduits, hemodynamic instability/ischemia and cardiogenic shock (9).
Worldwide Data
Recently a data was presented in American association of thoracic surgeons (AATS) annual meeting which stated that enthusiasm for OPCAB has vaned. The percentage of CABG’s performed off-pump has steadily declined over the last 5 years, and currently this technique is used in fewer than 1 in 5 patients who undergo CABG in the USA. A minority of surgeons and centers continue to perform OPCAB in most of their patients (10). Also in Europe about 25% of CABG procedures are performed off-pump (11).
However, the trend is quite opposite in Asian countries like Japan where approximately 60% of the revascularizations are done as OPCAB (12). In India, the trend is also towards OPCAB. In our institute, we are doing around 4,000 cardiac surgical procedures, majority of which are CABGs (75%) of which 80% are done as OPCAB.
OPCAB vs. CCAB
There is lot of ongoing debate about advantages of OPCAB over CCAB and vice versa. Proponents of OPCAB suggest decreased neurocognitive dysfunction by avoiding cannulation and aortic cross clamping, avoidance of SIRS, decreased blood and products use, better postoperative pulmonary and renal function as well as shorter length of stay (LOS) in intensive care unit (ICU) and hospital (13). Argument in favor of CCAB suggests complete revascularization and better long-term graft patency. Moreover, emergency conversion from OPCAB to CCAB does have higher morbidity and mortality (14). Minimally invasive approaches like minimally invasive direct CABG (MIDCAB) or total endoscopic CABG (TECAB) are performed without CPB, but, there are limitations associated with OPCAB like it is technically difficult, and subendocardial ischemia can occur during anastomosis leading to conversion to CCAB.
Review of literature revealed many randomized controlled trials (RCTs) comparing OPCAB or CCAB for graft patency, duration of ventilation, ICU and hospital LOS, perioperative morbidity and mortality as well as long term outcome.
Racz et al (15) studied approximately 68,000 patients from 1997 to 2000 undergoing CABG either OPCAB (n=9,135) or CCAB (n= 59,044) for short and long term outcomes like hospital mortality and complications, three-year risk adjusted mortality and mortality/revascularization. OPCAB patients had lower risk-adjusted mortality 2.02% vs. 2.16% (p=0.39), lower rates of perioperative stroke [1.6% vs. 2.0%, p< 0.003], bleeding requiring reoperation (1.6% vs. 2.2%, p<0.001) and lower postoperative LOS (median 5 days vs. 6 days, p<0.001). However, OPCAB had higher rates of gastrointestinal bleeding, perforation, or infarction (1.2% vs. 0.9%, p=0.003). On the other hand CCAB patients had better three-year survival [adjusted risk ratio (RR) =1.086, p=0.045] and better chances of freedom from death or revascularization (adjusted RR= 1.232, p<0.001). Moreover, an important observation they made was that OPCAB was technically more demanding and outcomes may improve as compared to CCAB in the future as more surgeons master the learning curve with improvements in methods for stabilization of the heart.
Later ROOBY (randomized on/off bypass) trial (16) studied 2203 patients in 18 centers undergoing elective or urgent OPCAB or CCAB. They found no significant difference in the rate of the 30-day composite outcome i.e. reoperation, new mechanical support, cardiac arrest, coma, stroke, or renal failure, (7.0% and 5.6%), respectively; p=0.19. There were lesser grafts in OPCAB and rate of graft patency was also lower in the OPCAB group (82.6% vs. 87.8%, p<0.01). They concluded that OPCAB was associated with poor graft patency as well as poor composite endpoint at 1 year follow-up. However, major limitations were gender bias (mostly males), surgeon bias (role of primary surgeon not defined) and high conversion rate to on pump.
A meta-analysis of 37 randomized trials (3,369 patients) by Cheng et al (17) revealed superiority of OPCAB with regard to atrial fibrillation (AF), inotropes requirement, blood transfusion, ventilation time, respiratory infections and LOS in ICU and hospital. They concluded that certain “short and midterm clinical and resource outcomes” improved with OPCAB. This is one of the few early papers that revealed the benefits of OPCAB over CCAB. Later, Puskas et al (18) in their meta-analysis on low as well as high risk patients also described the benefits of OPCAB in terms of morbidity, mortality, LOS in ICU and hospital, cognitive dysfunction and overall quality of life.
Recently, a multicentric CORONARY trial (19) involving 4,752 patients also revealed that there was no difference between two techniques with respect to the 30-day mortality, myocardial infarction, stroke, or renal failure requiring dialysis. Moreover, there was decreased transfusion requirement (50.7% vs. 63.3%; p<0.001) and reoperation for perioperative bleeding (1.4% vs. 2.4%; p=0.02) as compared to CCAB. There were less respiratory (5.9% vs. 7.5%; p=0.03) and renal complications (28.0% vs. 32.1%; p=0.01), however there was increased risk of early revascularization (0.7% vs. 0.2%; p=0.01) in OPCAB. In the same year, an editorial by Grover (20) discussed ROOBY and CORONARY trials and suggested that long-term data should be analyzed. The result of this data will address the controversial topics and specific subgroups of patients who might benefit from OPCAB.
We are practicing OPCAB since 1990’s and have vast experience with it in a variety of patients. We performed a retrospective analysis of 28,216 patients who underwent elective CABG over a 15-year period from 1990 to 2004 at our center. Isolated OPCAB was performed in 14,030 patients (21). The overall period was divided into 3 groups of 5 years each: Group I (1990-1994), Group II (1995-1999) and Group III (2000-2004). Initially, OPCAB was performed only in high-risk patients later on it was electively performed in 96-98% of CABG patients (2000-2004). Patients’ medical charts were reviewed for age, preoperative risk factors, operative findings, intraoperative conversion rate to CPB, postoperative complications, and hospital LOS. We found improvement in OPCAB in the number of grafts as compared to CCAB from the first (1990-1994) 2.0 ± 0.4 vs. 3.2 ± 0.8 to the third (2000-2004) period 3.5 ± 0.2 vs. 3.4 ± 0.8, conversion to CPB (5.2% vs. 1.7%), perioperative MI (5.2% vs. 1.5%), and hospital mortality (5.2% vs. 1.1%). Moreover LOS in ICU and hospital was shorter in group III as compared to group I. We concluded that the “learning curve” associated with OPCAB can be improved over time and careful selection of patients, is also important.
Another study from our group on 4953 patients who underwent OPCAB found decreased ventilation time (19 ± 4 hours vs. 25 ± 6 hours; p<0.001), blood loss (350 ± 41mL vs 598 ± 74mL; p<0.001), blood and blood products usage (30.8% vs. 45.3%; p<0.001) and rexploration for bleeding (0.6% versus 2.8%; p<0.001). Moreover there was decreased need for intraaortic balloon pump (IABP) (1.3% vs. 2.6%; p<0.001) and decreased mortality rate (0.97% vs. 1.86%; p<0.001) as well as decrease in ICU and hospital LOS in these patients (22).
OPCAB and High Risk Patients
In high risk patients i.e. the patients with poor left ventricular ejection fraction (LVEF ≤ 30%), age greater than 70 years, left main coronary artery stenosis, acute myocardial infarction, and redo coronary artery surgery, OPCAB is considered beneficial. We studied 1,075 consecutive high-risk patients who underwent OPAB and found better results as compared to CCAB with regard to hospital mortality 3.2% vs. 4.5% (p=0.109), intubation time (19 ± 5 vs. 24 ± 6 hours, p<0.001), mean blood loss (362 ± 53 vs. 580 ± 66 mL, p<0.001), atrial fibrillation (14.3 vs 19.7%, p<0.001) and ICU and hospital LOS (p<0.001). We concluded that OPCAB can be safely performed in high-risk patients with multivessel coronary artery disease (23). In patients with atheromatous aorta and with severe LV dysfunction we have shown better results with OPCAB (24,25). Moreover in patients having unstable angina OPCAB is also considered a safe technique (26).
A metaanalysis and consensus statement by International Society for minimally invasive cardiac surgery (ISMICS) published in 2005 stated that OPCAB was a safe alternative to CCAB with respect to mortality and morbidity (Class I, level A), completeness of revascularization and graft patency (Class IIa, Level A), quality of life (Class I, Level A) and cognitive dysfunction (Class IIa, Level A). Moreover, OPCAB also reduced the duration of ventilation, ICU and hospital LOS, had better resource utilization (Class I, Level A) and was beneficial in high-risk patients as well (Class IIa, Level B) (18).
Another meta-analysis (23 RCTs and 7,759 patients) in patients with LV dysfunction also revealed mortality benefit in OPCAB patients. Although it was associated with incomplete revascularization, however, that was not reflected in the clinical outcome (27).
OPCAB and Redo Surgery
Reoperative CABG has high mortality and morbidity and more chances of complications in the perioperative period. There are more chances of prolonged ventilation and ICU stay, increased blood requirement and postoperative infections. OPCAB is considered a safe technique for reoperative CABG. We studied 350 patients who underwent redo CABG either OPCAB (n=156) or CCAB (n=194) and found better outcomes in the former group (28,29). In OPCAB patients, there was decrease in postoperative blood transfusion (12.82% vs. 86.3%, p=0.001), decreased ventilatory support (>24 hours) (7.7% vs. 16.49%, p=0.021) and decreased inotropic requirement (10.89% vs. 23.71%, p=0.003). Moreover there was decreased ICU (20 ± 4.1 hours vs. 40 ± 6.2 hours, p=0.001) and hospital LOS (5 ± 3.4 days vs. 9 ± 4.2 days, p=0.001) and in-hospital mortality (3.2% vs. 7.7%, p=0.114) as well. We concluded that off-pump redo coronary artery bypass grafting was a safe technique of myocardial revascularization.
Recently a retrospective analysis from Japan cardiovascular surgery database on 34,980 patients who underwent isolated CABG (2008-2011) was done, out of which 1.8% (n=617/34980) patients underwent redo CABG. Redo surgery was primarily done as OPCAB in 364 (59%) and CCAB in 253 (41%). In redo OPCAB patients there was less mean operation time (353.7 vs. 441.3 min, p<0.0001), 30-day mortality rate (3.5 vs. 7.0%, p=0.18), composite mortality or major morbidities (11.0 vs. 21.5%, p=0.006), prolonged ventilation (>24 h) (7.0 vs. 15.0%, p=0.016), ICU LOS (≥8 days) (7.0 vs. 14.5%, p=0.023) and blood transfusions (71.5 vs. 94.0%, p<0.0001). They concluded that OPCAB reduced early operative mortality and the incidences of major complications in redo CABG (30).
Nowadays in the era of minimally invasive cardiac surgery, redo CABG can be performed through posterolateral thoracotomy. We have done a pilot study in a few patients with favorable results. In our patients angioplasty had failed and internal mammary artery graft was patent. Therefore, radial artery graft was used for vein graft to lateral wall through posterolateral thoracotomy, the proximal anastomosis being from the descending aorta.
Nowadays in the era of minimally invasive cardiac surgery, redo CABG can be performed through posterolateral thoracotomy. We have done a pilot study in a few patients with favorable results. In our patients angioplasty had failed and internal mammary artery graft was patent. Therefore, radial artery graft was used for vein graft to lateral wall through posterolateral thoracotomy, the proximal anastomosis being from the descending aorta.
OPCAB and Stroke
Stroke after cardiac surgery increases perioperative mortality and morbidity. The reported incidence of neurological complications after CCAB is 3-6%. Aortic manipulation (aortic cannulation or proximal anastomosis) during cardiac surgery in vulnerable patients may lead to perioperative stroke. OPCAB has been associated in recent studies with decreased morbidity and risk of perioperative stroke (31). Moreover, avoiding manipulation of aorta during OPCAB may also decrease the chances of perioperative neurological events. It has been revealed in a meta-analysis that in comparison to OPCAB without manipulation of aorta with CCAB the rate of stroke was 0.38% vs. 1.87% (p<0.0001) (32). In another study, in patients with left main disease (LMD) “clampless” OPCAB was associated with decreased incidence of stroke as compared to CCAB. (0.4% vs. 2.9%; p=0.012), particularly in patients with carotid artery disease and with previous history of stroke (33). In our experience also there has been less incidence of stroke rate with OPCAB (34).
OPCAB & Renal Dysfunction
Use of CPB may adversely affect renal function and occasionally results in renal failure following cardiac surgery. Avoidance of CPB may prevent the renal dysfunction in high risk patients like LV dysfunction, peripheral vascular disease, diabetes mellitus, emergent procedure, high body mass index (BMI) and on IABP support (35).
In dialysis dependent patients with end stage renal disease, OPCAB is considered as safe alternative to CCAB. In a study on 294 dialysis-dependent patients, 168 patients underwent OPCAB, with significantly less in-hospital mortality as compared to CCAB (5.4% vs. 11.9%, p=0.04) (36). The OPCAB technique has also been shown to preserve glomerular filtration rate (GFR) with lesser increase in creatinine levels and superior renal protection (37). Moreover, in an analysis on 7,42,909 CABG patients from Society of Thoracic Surgery database (2004-2009) with regard to in hospital mortality and need for renal replacement therapy (RRT), there was less incidence of death and RRT in OPCAB patients with known chronic kidney disease (CKD) (38).
In a recent multicentric study 2932 patients from CORONARY trial were enrolled into a kidney function substudy to record serum creatinine concentrations during the postoperative period and at 1 year. They found reduced risk of acute kidney injury (AKI) in postoperative period after OPCAB (39).
OPCAB & Percutaneous Coronary Intervention (PCI)
PCI with drug eluting stent (DES) has challenged CABG as the gold standard for multivessel CAD. However, there is still paucity of data to verify the same. Authors compared PCI with OPCAB in multivessel CAD and found better cumulative major adverse cardiac and cerebrovascular events (MACCE) and clinical outcome in one year follow-up. Moreover three-year survival rate and survival free from MACCE at 3 years were also better in OPCAB (99.5% ± 0.5% vs. 95.1% ± 2.9%, p=0.075) and (91.3% ± 2.9% vs. 73.3% ± 5.3%, p<0.001), respectively (40).
Recently in LMD, comparison of these techniques also favored OPCAB over PCI. OPCAB had decreased early mortality (0 vs 5%; p<0.001), better overall survival at 8 years (88.6 ± 3.5% vs. 85.8 ± 5.3%; p=0.394) and freedom from MACCE at 8 years (83.9 ± 5.1 vs. 60.2 ± 6.9%; p<0.001). However, the incidence of stroke was similar in both groups (41).
In comparison to PCI arm of Syntax trial, OPCAB was also found to be superior after three years follow-up in terms of MACCE (10.3% vs. 28.0%; p<0.001), repeat revascularization (4.3% vs. 19.7%; p<0.001) and stroke (1.3 vs. 2%; p=0.347) (42).
OPCAB - Gender and Body Habitus
Gender particularly female patients are considered as high risk for CABG in view of smaller target vessels and conduits and associated co-morbidities. Women have a poorer prognosis and a more unfavorable outcome than men after myocardial infarction or interventional procedures.
In a study on 3,500 patients who underwent CABG in India, 14.6% of patients were women in whom they found smaller coronary artery size than males even with body surface area >1.52 m2. In-hospital mortality was higher in females (2.92% vs. 1.8%) primarily due to low cardiac output and renal failure. However, interesting finding was association of OPCAB with reduced mortality (1.84% vs. 4.5%; p=0.01) in women, blood requirement (2.5 ± 1.2 units vs. 4.3 ± 1.4 units; p<0.001); ICU stay (29.4 ± 16.4 hours vs. 38.3 ± 17.3 hours; p<0.0001); and hospital LOS (6.81 ± 1.6 days vs. 8.05 ± 2.1 days; p<0.0001). However, there was no statistically significant difference in the rates of mediastinitis, arrhythmias, and neurological or pulmonary complications (43).
A meta-analysis of six observational studies involving 23313 patients (9596 OPCAB and 13717 CCAB) also revealed lesser 30-day mortality (4.8% vs. 0.7%; p=0.92) and decreased peri-operative myocardial infarction (p=0.0009) in OPCAB. They concluded that OPCAB is a safe alternative to CCAB in female patients (44). Apart from reducing in-hospital mortality, OPCAB in female patients also has lower rate of postoperative atrial fibrillation than male patients (6% vs. 15%; p=0.08) (45). A retrospective study on female patients undergoing CABG revealed CPB as an independent predictor and risk factor of increased early and midterm postoperative mortality in female gender. OPCAB significantly reduces early and midterm postoperative mortality in women and the authors recommended it as a preferred technique (46).
Patients who are morbidly obese and thin built are also considered as high risk for CABG. A study on 6801 patients undergoing CABG, BMI<25, 4312 (OPCAB, 2083; CCAB, 2229) and BMI>35, 2489 (OPCAB, 1127; CCAB, 1362) revealed advantages of OPCAB in the form of decreased in-hospital mortality (adjusted odds ratio, 0.48; 95% CI, 0.28-0.82), stroke (adjusted odds ratio, 0.31; 95% CI, 0.18-0.56), new-onset renal failure (adjusted odds ratio, 0.59; 95% CI, 0.36-0.96) and chances for prolonged ventilation (adjusted odds ratio, 0.50; 95% CI, 0.38-0.64) (47). We are routinely practicing OPCAB in morbidly obese patients and administering regional analgesia (thoracic epidural analgesia) for perioperative analgesia (48).
OPCAB and Elderly
Elderly (>70 years) coming for cardiac surgery are considered as high risk patients. Nowadays the population of this group coming for coronary revascularization is increasing. A multicenter, randomized trial ‘DOOR’ (Danish On-Pump Versus Off-Pump Randomization Study) on 900 patients > 70 years of age undergoing CABG was done to study combined end point of death, stroke, or myocardial infarction. They found both CCAB and OPCAB as safe procedures in elderly patients. No major differences in intermediate-term outcomes were found (49).
GOPCABE trial (German Off-Pump Coronary Artery Bypass Grafting in Elderly Patients) also compared OPCAB versus CCAB in elderly patients (>75years) (50). They found no significant difference with regard to the composite outcome of death, stroke, myocardial infarction, repeat revascularization, or new RRT within 30 days and within 12 months after surgery.
OPCAB- Other Advantages
In view of shorter duration of surgery, less heparinization and early mobilization, non-cardiac surgery can also be performed in the same sitting. We have also done combined procedures like thyroidectomy (51) in a patient with a huge goiter with respiratory obstruction. We also performed hip and knee joint replacement with OPCAB in the same sitting in a patient who was admitted for total knee replacement, found to have critical CAD and had a fall with fracture hip (52). OPCAB can also be performed safely in conditions with platelet dysfunction like dengue fever (53). OPCAB can be safely performed in combination with carotid endarterectomy as well (54).
Moreover, by avoiding CPB regional analgesia, particularly neuroaxial blocks, can be given in selected patients for better postoperative analgesia. We are routinely using these techniques in morbidly obese as well in patients with reactive airway disease (48,54-58).
OPCAB and SIRS
Complement activation, cytokine production, and related cellular responses are important factors during open-heart surgery. CPB activates the complement systems, thereby causing production of several inflammatory cytokines. OPCAB is associated with reduced postoperative rise in markers of SIRS, such as C3a, C5a, and TNF-α, or interleukin (IL)-6 and IL-8 (59). Elderly and poor left ventricular patients have shown increased levels of proinflammatory markers on CPB. Thus OPCAB is found to be beneficial in these patients (60). Recent study has shown attenuation of endothelin (ET) levels in patients undergoing OPCAB in systemic, pulmonary, and coronary circulation as well as lower levels of Neopterin, IL-6 and IL-8 (61,62).
OPCAB and Cost analysis
Apart from reducing the complications associated with CPB, OPCAB also reduces cost and helps in reducing resource utilization due to reduced disposable (CPB circuit and cannulae). Previously the cost advantage of OPCAB was offset due to risk of intraoperative conversions and they found that the cost increased exponentially if the probability of conversion was more than 15% (63). Authors also found it to be durable and cost-effective along with providing complete revascularization (64). In patients more than 70 years of age OPCAB is also considered to be more cost effective than CCAB (65).
Conclusion
OPCAB is a safe procedure for coronary revascularization. It may reduce risk of stroke, renal failure, atrial fibrillation, myocardial infarction, blood transfusion, and reduces duration of mechanical ventilation and LOS as well as the cost. Although it increases the risk of repeat revascularization after one year still it may be a “better” technique for high risk patients with major comorbidities, atheromatous aorta, LV dysfunction and redo surgery. However, large multicentric RCTs with longer follow-up are required to prove the same. However, the jury is still out.
References
References
1. Favaloro RG. Landmarks in the development of coronary artery bypass surgery. Circulation. 1998;98:466-78.
2. Epstein AJ, Polsky D, Yang F, Yang L, Groeneveld PW. Coronary revascularization trends in the United States, 2001-2008. JAMA. 2011;305:1769-76.
3. Menasché P. The systemic factor: the comparative roles of cardiopulmonary bypass and off-pump surgery in the genesis of patient injury during and following cardiac surgery. Ann Thorac Surg. 2001;72:S2260-6
4. Kolessov VI. Mammary artery-coronary artery anastomosis as a method of treatment for angina pectoris. J Thorac Cardiovasc Surg. 1967;54:535-44.
5. Arai H. Recent advancement in devices for off-pump coronary artery bypass grafting. Ann Thorac Cardiovasc Surg. 2007;13:1-4.
6. Bergsland J, Karamanoukian HL, Soltoski PR, Salerno TA. `Single suture’ for circumflex exposure in off-pump coronary artery bypass grafting. Ann Thorac Surg. 1999;68:1428-30.
7. Subramanian VA, McCabe JC, Geller CM. Minimally invasive direct coronary artery bypass grafting: two-year clinical experience. Ann Thorac Surg. 1997;64:1648–55.
8. Baumgartner FJ, Gheissari A, Capouya ER, Panagiotides GP, Katouzian A, Yokoyama T. Technical aspects of total revascularization in off-pump coronary bypass via sternotomy approach. Ann Thorac Surg 1999;67:1653-8.
9. Puskas JD, Wright CE, Ronson RS, Brown WM 3rd, Gott JP, Guyton RA. Off-pump multivessel coronary bypass via sternotomy is safe and effective Ann Thorac Surg. 1998;66:1068–72.
10. Chassot PG, van der Linden P, Zaugg M, Mueller X M, Spahn DR. Off-pump coronary artery bypass surgery: physiology and anaesthetic management. British Journal of Anaesthesia. 2004;92:400-13.
11. Afilalo J, Rasti M, Ohayon SM, Shimony A, Eisenberg MJ. Off-pump vs. on-pump coronary artery bypass surgery: an updated meta-analysis and meta-regression of randomized trials. Eur Heart J. 2012;33:1257–67.
12. Sakata R, Fujii Y, Kuwano H. Thoracic and cardiovascular surgery in Japan during 2008. Annual report by the Japanese Association for Thoracic Surgery. Gen Thorac Cardiovasc Surg. 2010;58:356-83.
13. Mehta Y, Juneja R. Off-pump coronary artery bypass grafting: new developments but a better outcome? Curr Opin Anaesthesiol. 2002;15:9-18.
14. Li Z, Amsterdam EA, Danielsen B, Hoegh H, Young JN, Armstrong EJ. Intraoperative conversion from off-pump to on-pump coronary artery bypass is associated with increased 30-day hospital readmission. Ann Thorac Surg. 2014;98:16-22.
15. Racz MJ, Hannan EL, Isom OW, Subramanian VA, Subramanian VA, Jones RH, Gold JP, Ryan TJ, Hartman A, Culliford AT, Bennett E, Lancey RA, Rose EA. A comparison of short- and long-Term outcomes after off-pump and on-pump coronary artery bypass graft surgery with sternotomy. J Am Coll Cardiol. 2004;43:557–64.
16. Shroyer AL, Grover FL, Hattler B, Collins JF, McDonald GO, Kozora E, Lucke JC, Baltz JH, Novitzky D; Veterans Affairs Randomized On/Off Bypass (ROOBY) Study Group. On-Pump versus Off-Pump Coronary-Artery Bypass Surgery. N Engl J Med. 2009;361:1827-37.
17. Cheng DC, Bainbridge D, Martin JE, Novick RJ. Does off-pump coronary artery bypass reduce mortality, morbidity, and resource utilization when compared with conventional coronary artery bypass? A meta-analysis of randomized trials. Anesthesiology. 2005;102:188-203.
18. Puskas J, Cheng D, Knight J, Angelini G, Decannier D, Diegeler A, Dullum M, Martin J, Ochi M, Patel N, Sim E, Trehan N, Zamvar V. Off-Pump versus conventional coronary artery bypass grafting: A meta-analysis and consensus statement from the 2004 ISMICS consensus conference. Innovations (Phila). 2005;1:3-27
19. Lamy A, Devereaux PJ, Prabhakaran D, Taggart DP, Hu S, Paolasso E, Straka Z, Piegas LS, Akar AR, Jain AR, Noiseux N, Padmanabhan C, Bahamondes JC, Novick RJ, Vaijyanath P, Reddy S, Tao L, Olavegogeascoechea PA, Airan B, Sulling TA, Whitlock RP, Ou Y, Ng J, Chrolavicius S, Yusuf S; CORONARY Investigators. Off-pump or on-pump coronary-artery bypass grafting at 30 days. N Engl J Med. 2012;366:1489-97.
20. Grover FL. Current status of off-pump coronary-artery bypass. N Engl J Med. 2012;19;366:1541-3.
21. Mishra YK, Mishra M, Malhotra R, Meharwal ZS, Kohli V, Trehan N.
Evolutions of off-pump coronary artery bypass grafting over 15 years: A single-institution experience of 14,030 cases. Innovations. 2005;1:88-91.
22. Meharwal ZS, Mishra YK, Kohli V, Singh S, Bapna RK, Mehta Y, Trehan N. Multivessel off-pump coronary artery bypass: analysis of 4953 cases. Heart Surg Forum. 2003;6:153-9.
23. Meharwal ZS, Mishra YK, Kohli V, Bapna R, Singh S, Trehan N. Off-pump multivessel coronary artery surgery in high-risk patients. Ann Thorac Surg. 2002;74:S1353-7.
24. Mishra M, Malhotra R, Karlekar A, Mishra Y, Trehan N. Propensity case-matched analysis of off-pump versus on-pump coronary artery bypass grafting in patients with atheromatous aorta. Ann Thorac Surg. 2006;82:608-14.
25. Meharwal ZS, Trehan N. Off-pump coronary artery bypass grafting in patients with left ventricular dysfunction. Heart Surg Forum. 2002;5:41-5
26. Kohli V, Goel M, Sharma VK, Mishra Y, Malhotra R, Mehta Y, Trehan N. Off-pump surgery: a choice in unstable angina. Asian Card thorac Annals. 2003;11:285-8
27. Jarral OA, Saso S, Athanasiou T. Off-pump coronary artery bypass in patients with left ventricular dysfunction: a meta-analysis. Ann Thorac Surg. 2011;92:1686-94.
28. Mishra Y, Wasir H, Kohli V, Meharwal ZS, Bapna R, Mehta Y, Trehan N. Beating heart versus conventional reoperative coronary artery bypass surgery. Indian Heart J. 2002;54:159-63.
29. Mishra YK, Collison SP, Malhotra R, Kohli V, Mehta Y, Trehan N. Ten-year experience with single-vessel and multivessel reoperative off-pump coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2008;135:527-32.
30. Dohi M, Miyata H, Doi K, Okawa K, Motomura N, Takamoto S, Yaku H; Japan Cardiovascular Surgery Database. The off-pump technique in redo coronary artery bypass grafting reduces mortality and major morbidities: propensity score analysis of data from the Japan Cardiovascular Surgery Database. Eur J Cardiothorac Surg. 2015;47:299-307; discussion 307-8.
31. Bowles BJ, Lee JD, Dang CR, Taoka SN, Johnson EW, Lau EM, Nekomoto K. Coronary artery bypass performed without the use of cardiopulmonary bypass is associated with reduced cerebral microemboli and improved clinical results. Chest 2001;119:25-30.
32. Edelman JJ, Yan TD, Bannon PG, Wilson MK, Vallely MP. Coronary artery bypass grafting with and without manipulation of the ascending aorta--a meta-analysis. Heart Lung Circ. 2011;20:318-24.
33. Emmert MY, Salzberg SP, Seifert B, Scherman J, Plass A, Starck CT, Theusinger O, Hoerstrup SP, Grünenfelder J, Jacobs S, Falk V. Clampless off-pump surgery reduces stroke in patients with left main disease. Int J Cardiol. 2013;167:2097-101.
34. Trehan N, Mishra M, Kasliwal RR, Mishra A. Reduced neurological injury during CABG in patients with mobile aortic atheromas: a five-year follow-up study. Ann Thorac Surg. 2000;70:1558-64.
35. Gu TX, Zhang WF, Xiu ZY, Fang Q, Zhang YH, Wang C. Incidence and risk factors of acute kidney injury post off-pump and on-pump coronary artery bypass grafting. [Article in Chinese] Zhonghua Xin Xue Guan Bing Za Zhi. 2008;36:1092-6.
36. Zhang L, Boyce SW, Hill PC, Sun X, Lee A, Haile E, Garcia JM, Corso PJ. Off-pump coronary artery bypass grafting improves in-hospital mortality in patients with dialysis-dependent renal failure. Cardiovasc Revasc Med. 2009;10:12-6.
37. Hayashida N, Teshima H, Chihara S, Tomoeda H, Takaseya T, Hiratsuka R, Shoujima T, Takagi K, Kawara T, Aoyagi S. Does off-pump coronary artery bypass grafting really preserve renal function? Circ J. 2002;66:921-5.
38. Chawla LS, Zhao Y, Lough FC, Schroeder E, Seneff MG, Brennan JM. Off-pump versus on-pump coronary artery bypass grafting outcomes stratified by preoperative renal function. J Am Soc Nephrol. 2012;23:1389-97.
39. Garg AX, Devereaux PJ, Yusuf S, Cuerden MS, Parikh CR, Coca SG, et al. Kidney function after off-pump or on-pump coronary artery bypass graft surgery. JAMA. 2014;311:2191-8.
40. Yi G, Youn YN, Yoo KJ, Hong YS. Comparison of off-pump coronary artery bypass grafting with percutaneous coronary intervention versus drug-eluting stents for three-vessel coronary artery disease. Ann Thorac Surg. 2008;86:1438-43.
41. Jeong DS, Lee YT, Chung SR, Jeong JH, Kim WS, Sung K, Park PW. Revascularization in left main coronary artery disease: comparison of OPCAB vs PCI. Eur J Cardiothorac Surg. 2013;44:718-24.
42. Arrigoni SC, Mecozzi G, Grandjean JG, Hillege JL, Kappetein AP, Mariani MA. Off-pump no-touch technique: 3-year results compared with the SYNTAX trial. Interact Cardiovasc Thorac Surg. 2015 Feb 7. pii: ivv012. [Epub ahead of print]
43. Yadava OP, Prakash A, Kundu A, Yadava M. Coronary artery bypass grafting in women--is OPCAB mandatory? Indian Heart J. 2011;63:425-8.
44. Attaran S, Harling L, Ashrafian H, Moscarelli M, Casula R, Anderson J, Punjabi P, Athanasiou T. Off-pump versus on-pump revascularization in females: a meta-analysis of observational studies. Perfusion. 2014;29:385-96.
45. Bernet F, Baykut D, Reineke D, Matt P, Zerkowski HR. Impact of female gender on the early outcome in off-pump coronary artery bypass surgery. Eur J Med Res. 2006;11:114-8.
46. Eifert S, Kilian E, Beiras-Fernandez A, Juchem G, Reichart B, Lamm P. Early and midterm mortality after coronary artery bypass grafting in women depends on the surgical protocol: retrospective analysis of 3441 on- and off-pump coronary artery bypass grafting procedures. J Cardiothorac Surg. 2010;5:90
47. Keeling WB, Kilgo PD, Puskas JD, Halkos ME, Lattouf OM, Guyton RA, Thourani VH. Off-pump coronary artery bypass grafting attenuates morbidity and mortality for patients with low and high body mass index. J Thorac Cardiovasc Surg. 2013;146:1442-8
48. Sharma M, Mehta Y, Sawhney R, Vats M, Trehan N. Thoracic epidural analgesia in obese patients with body mass index of more than 30 kg/m2 for off pump coronary artery bypass surgery. Ann Card Anaesth. 2010;13:28-33.
49. Houlind K, Kjeldsen BJ, Madsen SN, Rasmussen BS, Holme SJ, Nielsen PH, Mortensen PE; DOORS Study Group. On-Pump versus off-pump coronary artery bypass surgery in elderly patients-Results from the Danish on-pump versus off-pump randomization study. Circulation. 2012;125:2431-9.
50. Diegeler A, Börgermann J, Kappert U, Breuer M, Böning A, Ursulescu A, Rastan A, Holzhey D, Treede H, Rieß FC, Veeckmann P, Asfoor A, Reents W, Zacher M, Hilker M; GOPCABE Study Group. Off-pump versus on-pump coronary-artery bypass grafting in elderly patients. N Engl J Med. 2013;368:1189-98.
51. Mehta Y, Juneja R, Singh H, Sachdeva S, Trehan N. OPCAB and thyroidectomy in a patient with a severely compromised airway. J Cardiothorac Vasc Anesth. 2005;19:79-82.
52. Mehta Y, Sujatha P, Rajgopal A, Meharwal Z S, Trehan N. Off pump CABG along with hip & knee replacement: Anesthetic management. J Anaesth Clin Pharmacol. 2005;21:445-7.
53. Rawat SK, Mehta Y, Trehan N. CABG in a patient recovering from dengue fever. Indian Heart J. 2009;61:386-8.
54. Mishra Y, Mehta Y, Trehan N. Concomitant carotid endarterectomy and coronary bypass surgery: outcome of on-pump and off-pump techniques. Ann Thorac Surg. 2004;78:2037-42; discussion 2042-2043.
55. Mehta Y, Swaminathan M, Mishra Y, Trehan N. A comparative evaluation of intrapleural and TEA for postoperative pain relief after MIDCAB surgery. J Cardiothorac Vasc Anesth. 1998;12:162-5.
56. Dhole S, Mehta Y, Saxena H, Juneja R, Trehan N. Comparison of continuous thoracic epidural and paravertebral blocks for postoperative analgesia after minimally invasive direct coronary artery bypass surgery. J Cardiothorac Vasc Anesth. 2001;15:288-92.
57. Mehta Y, Vats M, Sharma M, Arora R, Trehan N. Thoracic epidural analgesia for off-pump coronary artery bypass surgery in patients with chronic obstructive pulmonary disease. Ann Card Anaesth. 2010;13:224-30.
58. Mehta Y, Arora D, Sharma KK, Mishra Y, Wasir H, Trehan N. Comparison of continuous thoracic epidural and paravertebral block for postoperative analgesia after Robotic- assisted coronary artery bypass surgery. Ann Card Anaesth. 2008;11:90-5.
59. Matata BM, Sosnowski AW, Galinanes M. Off-pump bypass graft operation significantly reduces oxidative stress and inflammation. Ann Thorac Surg. 2000;69:785-91.
60. te Velthuis H, Jansen PG, Oudemans-van Straaten HM, Sturk A, Eijsman L, Wildevuur CR. Myocardial performance in elderly patients after cardiopulmonary bypass is suppressed by tumor necrosis factor. J Thorac Cardiovasc Surg. 1995;110:1663-9.
61. Unić D, Barić D, Brkić K, Planinc M, Jonjić D, Rudež I, Sutlić Ž.Off-pump myocardial revascularization attenuates endothelin-1 expression in systemic, pulmonary, and coronary circulation. Wien Klin Wochenschr. 2014;126:710-7.
62. Uyar IS, Onal S, Uysal A, Ozdemir U, Burma O, Bulut V. Evaluation of systemic inflammatory response in cardiovascular surgery via interleukin-6, interleukin-8, and neopterin. Heart Surg Forum. 2014;17:E13-7.
63. Shiga T, Apfel CC, Wajima Z, Ohe Y. Influence of intraoperative conversion from off-pump to on-pump coronary artery bypass grafting on costs and quality of life: a cost-effectiveness analysis. J Cardiothorac Vasc Anesth. 2007;21:793-9.
64. Puskas JD, Williams WH, Mahoney EM, Huber PR, Block PC, Duke PG, Staples JR, Glas KE, Marshall JJ, Leimbach ME, McCall SA, Petersen RJ, Bailey DE, Weintraub WS, Guyton RA. Off-pump vs conventional coronary artery bypass grafting: early and 1-year graft patency, cost, and quality-of-life outcomes: a randomized trial. JAMA. 2004;291:1841-9.
65. Houlind K, Kjeldsen BJ, Madsen SN, Rasmussen BS, Holme SJ, Pallesen PA, et al; DOORS Study Group. OPCAB surgery is cost-effective for elderly patients. Scand Cardiovasc J. 2013;47:185-92.
- Why Publish with JCPC?
- Instructions to the Authors
- Submit Manuscript
- Advertise with Us
- Journal Scientific Committee
- Editorial Policy
Print: ISSN: 2250-3528


