The Journal of Clinical and Preventive Cardiology has moved to a new website. You are currently visiting the old
website of the journal. To access the latest content, please visit www.jcpconline.org.
Student's Page
Intra-aortic Balloon Counter Pulsation
Volume 2, Jan 2013
Rahul Mehrotra MD, DNB Gurgaon, India
J Clin Prev Cardiol. 2013;2(1):55-7
Intra-aortic balloon pump (IABP) is a temporary mechanical circulatory assist device. It consists of a sausage-shaped balloon mounted on a catheter and placed in the descending thoracic aorta. By inflating during diastole and deflating during systole, it results in augmentation of the diastolic perfusion pressure and systolic unloading. The overall effects are an increased coronary perfusion, reduction in myocardial ischemia, reduced preload, afterload and myocardial oxygen demand, increased cardiac output, and peripheral perfusion. Due to these remarkable hemodynamic changes the device is very useful in situations requiring circulatory support in the presence of ischemic/failing heart.Indications
Registry data from the SHOCK trial (SHould we emergently revascularise Occluded coronaries for Cardiogenic shocK) suggested that in patients with acute myocardial infarction (MI) who received thrombolytic therapy, use of IABP support resulted in reduced hospital mortality compared to the patients in whom thrombolytic therapy alone was used (47% vs. 63%; p<0.0001) (1). Since then, the guidelines on acute MI (ACC/AHA as well as the ESC) recommend that IABP should be used in patients of acute infarction in whom cardiogenic shock cannot be quickly reversed with pharmacologic therapy (class I indication). Other appropriate indications for the use of IABP are shown in Table 1.
.jpg)
Apart from these class I indications, IABP is also used in high-risk patients undergoing percutaneous coronary interventions, although this has not shown to be of any benefit in clinical trials (2).
.jpg)
Apart from these class I indications, IABP is also used in high-risk patients undergoing percutaneous coronary interventions, although this has not shown to be of any benefit in clinical trials (2).
Complications
Although balloon counterpulsation is very useful in select situations, as mentioned above, it is also associated with certain complications which should be watched for and either avoided or detected early. The complications are mainly related to the access site in the femoral artery, or sometimes due to the effect of large bore catheter dwelling in the arterial system. In the Benchmark Counterpulsation Outcomes Registry, the incidence of major complications was 2.6% while that of the minor complications was 4.2% (3).Thorough understanding of the insertion technique, sizing, placement and monitoring is necessary to avoid the complications arising due to improper positioning, timing of inflation–deflation and peripheral limb ischemia. Table 2 lists the complications associated with the use of IABP. In general, the complications are more common in women, people with short stature and in the elderly.
.jpg)
Contraindications
IABP should not be inserted in patients with severe peripheral vascular disease, bleeding diathesis, severe
sepsis, suspected or known aortic dissection, sizable aortic aneurysms of aorta, significant aortic regurgitation
and in the presence of bilateral femoral-popliteal bypass grafts. Patients with end-stage cardiac disease who are not candidates for left ventricular assist device or cardiac transplant should also not be put on IABP.
Equipment, Insertion Technique and Monitoring
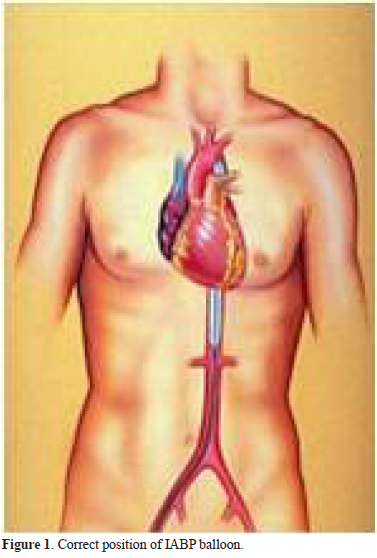
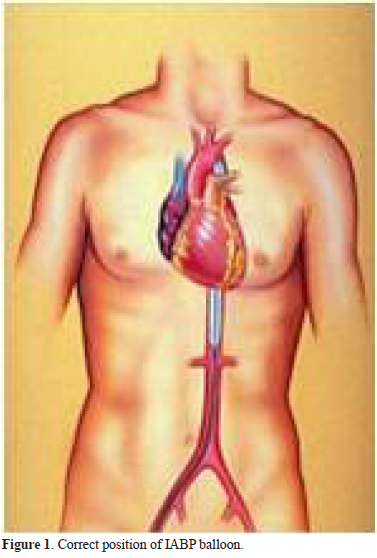
The device essentially consists of a console, a pump, helium cylinder, computer (all encased and mounted on a mobile trolley), which operates a catheter-mounted polyethylene balloon connected to it by tubing. The polyethylene balloon catheter has two lumens – one connected to helium pump for inflating and deflating it while the other opens out and is used to pass the catheter over a guide wire and later on, to monitor the central aortic pressure. The balloon size is chosen according to the patient’s height. Balloons are available from 25 to 50 cc capacities and the size of 40 cc is most commonly used since it is appropriate for people with height ranging from 5 feet to 5 feet 4 inches. The catheter with balloon is most commonly inserted via the common femoral artery using Seldinger technique but axillary, brachial cutdown and directly in the aorta (during surgery) approaches can also be used. Care should be taken to keep the tip of the balloon 1–2 cm distal to the origin of left subclavian artery and the other end proximal to renal arteries (Figure 1). The tip position can be located immediately after insertion on a chest X-ray (at the level of second rib) or if inserted in the cath lab, by fluoroscopy. The central lumen is connected to pressure transducer after flushing with heparin to display the aortic pressure tracing. Heparin bolus is given followed by an infusion to keep an activated partial thromboplastin time (APTT) of 60–80 seconds. The balloon inflations are synchronized according to the heartbeat depending on the requirement. Options are available to augment every beat, every other beat (1:2) or even up to 1 in 8 beats (usually required during weaning off).
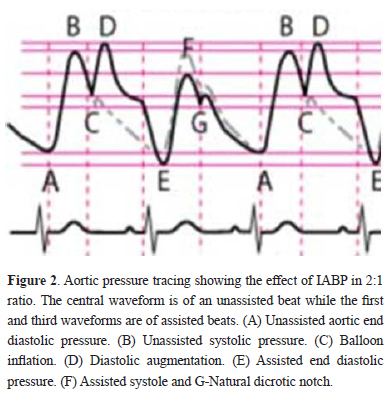
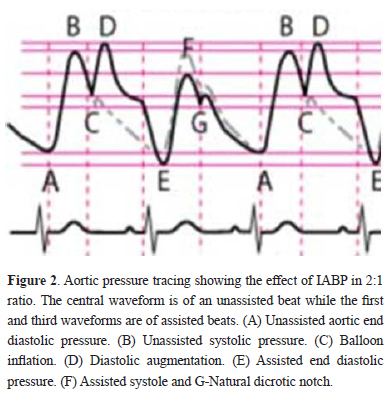
The most important aspect of the IABP is the inflation–deflation timing in relation to cardiac cycle since improper timing can result not only in lack of any benefit but also in hemodynamic deterioration. The balloon is timed to inflate at the onset of diastole with the closure of the aortic valve, marked by dicrotic notch on the aortic pressure trace (Figure 2). This results in augmentation of the diastolic pressure (D) and increased coronary and peripheral perfusion. The balloon remains inflated throughout diastole and is timed to deflate rapidly at the onset of systole (E). Rapid deflation of the balloon in aorta creates a dead space and a low-end diastolic pressure. This results in reduced afterload (F), reduced myocardial oxygen consumption and increased cardiac output. As shown in the figure, proper timing should ensure that D is greater than B, resulting in increased coronary perfusion while A is more than E resulting in decreased afterload and myocardial oxygen demand (B>F). As shown in the figure, C should be greater than G by about 5 mmHg indicating that the balloon should inflate just before dicrotic notch. Most machines have the option of setting the timings manually or choosing it automatically with ECG or pressure trace triggering. In case of arrhythmia, it is best to set the timing with ECG trigger.
The IABP should not be kept indwelling for long durations to prevent complications and should be gradually weaned off to allow time for hemodynamic adjustment in the patient.
To conclude, IABP is a useful mechanical assist device that is widely available and easy to use. Although clinical trials and meta-analysis in the recent times have failed to show any significant benefit, it is likely to be recommended to patients on an individual basis in the guidelines. Thorough understanding of its insertion technique, interpretation of waveforms and complications is essential to derive maximum benefit.
References
- Sanborn TA, Sleeper LA, Bates ER, Jacobs AK, Boland J, French JK, Dens J, Dzavik V, Palmeri ST, Webb JG, Goldberger M, Hochman JS. Impact of thrombolysis, intra-aortic balloon pump counter pulsation, and their combination in cardiogenic shock complicating acute myocardial infarction: a report from the SHOCK trial registry. SHould we emergently revascularise Occluded coronaries for Cardiogenic shocK? J Am Coll Cardiol. 2000;36(3 Suppl A):1123–9.
- Perera D, Stables R, Thomas M, Booth J, Pitt M, Blackman D, de Belder A, Redwood S; BCIS-1 Investigators. Elective intra-aortic balloon counter pulsation during high-risk percutaneous coronary intervention: a randomized controlled trial. JAMA. 2010;304:867–74.
- Barron HV, Every NR, Parsons LS, Angeja B, Goldberg RJ, Gore JM, Chou TM; Investigators in the National Registry of Myocardial Infarction 2. The use of intra-aortic balloon counterpulsation in patients with cardiogenic shock complicating acute myocardial infarction: data from the National Registry of Myocardial Infarction. Am Heart J. 2001;141:933–9.
- Why Publish with JCPC?
- Instructions to the Authors
- Submit Manuscript
- Advertise with Us
- Journal Scientific Committee
- Editorial Policy
Print: ISSN: 2250-3528


