The Journal of Clinical and Preventive Cardiology has moved to a new website. You are currently visiting the old
website of the journal. To access the latest content, please visit www.jcpconline.org.
Review Article
Hypertension in Pregnancy: Current Perspective
Volume 2, Apr 2013
Rahul Mehrotra MD, DNB, Ravi R Kasliwal MD, DM, Gurgaon, India
J Clin Prev Cardiol 2013;2(2):84-90
Introduction
Hypertension is the most common medical problem encountered during pregnancy worldwide. It is believed that hypertensive disorders complicate 5-10% pregnancies, depending upon the population studied and about 25% of all antenatal admissions are due to hypertension related complications (1). It is also considered to be the second most frequent cause of direct maternal death in the developed world (2). It is more common in the blacks, women more than 45 years of age and with diabetes. With the increasing trend of delaying pregnancy, increasing prevalence of baseline hypertension, diabetes and obesity, it is believed that these rates may actually be an underestimation of the true disease burden in the current era.
Hypertensive disorders in pregnancy remain a major cause of morbidity and mortality in the mother, the fetus and in the neonate. Pregnant women with hypertension suffer from complications such as abruptio placentae, intracerebral haemorrhage, disseminated intravascular coagulation, preeclampsia syndrome and multiorgan failure while the fetus is at risk of intrauterine growth retardation, prematurity, stillbirth and intrauterine death (3).
A thorough understanding of the various aspects of hypertensive disorders in pregnancy is essential as optimum management can result in favorable outcome of pregnancy with healthy mother and a healthy child.
We discuss here the physiology, the technique for detection and management of hypertension in pregnancy.
Physiology of Blood Pressure (BP) During Pregnancy
Maternal cardiovascular system undergoes numerous changes that progress continuously due to the changing patterns of circulatory hormones during pregnancy and labor. There is an increase in heart rate, circulating blood volume and thus cardiac output while there is a fall in peripheral vascular resistance. This results in a fall in the blood pressure. The fall in BP commences during the first trimester of pregnancy (by about seven weeks), and continues progressively to reach a nadir at about 20-24 weeks. The fall in diastolic BP is more (8-15mmHg) as compared to systolic BP (4-6 mmHg). As a result, the pulse pressure widens and the mean BP falls by about 6-10 mmHg. The exact etiology of these changes is not known clearly but they are believed to occur due to a combination of maternal and fetal factors. Increased production of vasodilator hormones like prostaglandins and nitric oxide; increased heat production by the fetus and generation of a low resistance vascular bed in the uterus are believed to be the chief mediators of these changes.
However, the blood pressure begins to rise thereafter and reaches the pregestational values by full term. Immediately after delivery, the BP usually falls again, but rises over the first week or so, sometimes causing transient hypertension even in women who had a normal BP throughout pregnancy (perhaps owing to vasomotor instability seen during this period).
These changes in blood pressure are seen in normotensive as well as in hypertensive women who become pregnant (4). The fall in BP in the first trimester is however, more pronounced in the latter and has several important implications, as discussed later.
BP Measurement During Pregnancy
Ideally, blood pressure in a pregnant woman should be measured in sitting position with the arm resting at the level of heart. However, it has been shown that the BP recorded in left arm in the left lateral recumbent position does not differ significantly from the values recorded in the sitting position. Therefore, the left lateral recumbent position is a reasonable alternative to the sitting position, especially in situations where it is not possible to make the patient sit up (during labor).
Mercury sphygmomanometer remains the gold standard (5) for measuring blood pressure during pregnancy and elevated BP readings should be confirmed on two separate occasions. Automatic devices for BP measurement are not recommended during pregnancy as they have not been shown to be reliable and differences to the tune of 15 mmHg have been reported when compared to mercury sphygmomanometer derived readings. Besides, automatic devices consistently underestimate BP in conditions like pre-eclampsia.
Systolic BP during pregnancy is denoted by appearance of sounds while deflating the cuff (Korotkoff I sound). There was considerable controversy and confusion regarding diastolic BP related to the use of Korotkoff phase IV (muffling) and V (disappearance of sounds) during pregnancy but now it has been recommended that Phase V should be used to denote DBP. This is because several studies have confirmed that phase V is more close to true intra-arterial BP, is easier to detect, reproducible and is rarely very low or close to zero. Phase IV (muffling of sounds) should be taken as the DBP value only in the rare situation where Korotkoff sounds persist even as the mercury level approaches zero (6).
Recently, the role of ambulatory BP measurement (ABPM) has been studied in pregnancy and it has been shown that ABPM is very useful in detection of white coat hypertension, a condition quite common in pregnant women. Also, hypertension in pregnancy as diagnosed by ABPM is a better predictor of unfavorable outcomes of pregnancy like low birth weight, proteinuria and pre-term delivery as compared to office based BP measurements (7). As of now, ABPM is not routinely recommended but it may be a useful technique for close supervision in high risk pregnancies, like the ones with hypertension and nephropathy (8).
Definition and Classification of Hypertension During Pregnancy
Systolic BP ≥ 140 mmHg and or a DBP ≥ 90 mmHg is considered to be the cutoff value for diagnosis of hypertension during pregnancy using appropriate technique as mentioned above (9). The terms like pre-hypertension or stages of hypertension are not used in this situation. It is also not advisable to use the terms like mild or severe hypertension since the complications related to hypertension in pregnancy (eclampsia) are not usually related to the severity of hypertension.
Several different classifications have been proposed by different authorities and societies over the years. This is a reflection of the poor understanding and scarce data related to this entity. There is however, general agreement on defining two broad categories- preexisting or gestational hypertension and looking for features of significant proteinuria to identify the pregnancy specific disease-Preeclampsia. This simplified classification was first proposed by the Canadians in 2008 and more recently a similar classification has been proposed by the European society of Cardiology in 2011 (10).
According to the ESC guidelines, hypertension in pregnancy is classified into 4 categories:
Chronic hypertension
- Pre existing or chronic hypertension
- Gestational hypertension
- Preeclampsia/Eclampsia
- Preeclampsia superimposed on chronic hypertension
Chronic hypertension
It is present when BP ≥140/90 mmHg is known to be present before pregnancy, before 20 weeks of gestation or persists beyond 42 days post partum. This type of hypertension complicates up to 5% of pregnancies but the incidence is rising due to the increasing trend of delaying pregnancy into later ages and increased prevalence of hypertension in younger individuals. An interesting caveat associated with this type of hypertension is that it may commonly be missed during the first trimester since the BP values normally dip during this time, as discussed earlier. This type of hypertension usually persists for more than 42 days after delivery and may or may not be associated with proteinuria.
Gestational hypertension
Also called pregnancy induced hypertension; it develops after 20 weeks of gestation and resolves within 42 days post partum. It is the commonest variety complicating 6-7% of pregnancies and can be associated with proteinuria.
Preeclampsia
This is a syndrome of gestational hypertension in association with significant proteinuria (>300mg protein in a 24 hour urine collection or >30 mg/ mmol in a spot urine sample. Pre-eclampsia remains one of the most common causes of maternal death worldwide. It is a pregnancy specific syndrome complicating about 5% of pregnancies. Women with obesity, diabetes, renal disease, collagen vascular disease and those belonging to low socioeconomic strata are also more prone to develop pre-eclampsia. Edema was earlier a part of the diagnostic criteria but is no longer included since it is extremely common, non-specific finding in pregnancy. Pre-eclampsia is associated with generalized hypo-perfusion as a result of endothelial dysfunction, vasospasm, and hypercoagulable state, forming microthrombi in the vasculature. The fetus suffers from placental hypo perfusion, intrauterine growth retardation and pre-mature delivery (11). In view of its detrimental effects on the pregnant mother and the fetus, pre-eclampsia should be suspected and looked for in vulnerable populations and managed appropriately. It is useful to remember that proteinuria is often a late manifestation and in pregnant women with new onset hypertension who complain of headache, flank pain, visual disturbances or have thrombocytopenia and altered liver enzymes, preeclampsia should be suspected (12). Eclampsia is the occurrence of seizures in a pregnant woman with preeclampsia.
Preeclampsia superimposed on chronic hypertension
In this condition, pregnant women who are hypertensive even before pregnancy develop further elevation of BP and features diagnostic of preeclampsia after 20 weeks of gestation. This can occur in up to 20-25% of pregnant women with chronic hypertension.
Evaluation and Management of Hypertension During Pregnancy
The general idea of evaluation in a pregnant woman with hypertension is to detect preeclampsia since it is a devastating entity associated with significant morbidity and mortality. A thorough history aimed at the risk factors for preeclampsia should be taken in all patients. Maternal features like nulliparity, advanced age (greater than 40 years), inter-pregnancy interval of less than 2 years or longer than 10 years are risk factors for preeclampsia. Similarly, history of preeclampsia or gestational hypertension in previous pregnancy, chronic hypertension, obesity, diabetes, chronic kidney disease, thrombophilia and systemic lupus erythematosus (SLE), are known predisposing conditions for preeclampsia. BP should be recorded meticulously at every antenatal visit in all patients.
In pregnant women detected to have hypertension, the type of hypertension, severity and target organ damage should be assessed. Laboratory tests like-complete hemogram (including hematocrit and platelet counts), liver function tests, kidney function tests, urine examination including detection of proteinuria with dipstick method should be done in all patients. If dipstick test is positive for proteinuria, 24 hour urine collection with estimation of proteinuria should be done. Even if dipstick test is negative in presence of risk factors of preeclampsia, 24 hour urine collection and protein estimation is useful since dipstick test has high false negativity.
Routine ultrasound abdomen and estimation of catecholamine in urine to screen for phaeochromocytoma has been recommended by few (13) but considering the rarity of the tumor and the cost of investigations, is not feasible in a country like ours and appears impractical.
Management of Hypertension
As opposed to hypertension in non-pregnant population, where large numbers of drugs are available with numerous, large scale trials to back them, there is very limited information and few drugs that can be safely used in pregnant women with hypertension. As discussed previously, the pregnant woman has altered cardiovascular physiology and the safety of the fetus has also to be accounted for. It is thus quite difficult to perform clinical trials in this population subset. It is not surprising then that, there has been no good quality clinical trial with adequate numbers involving this population group for the last more than 25 years now! The trial involving α Methyl Dopa and having an infant follow up of 7.5 years was published way back in 1976 (14). Most of the other trials have been small, with different ethnic groups, with inadequate follow-up and flawed designs. Thus, it should be remembered that most of the antihypertensive drugs have insufficient database to back their use in pregnancy.
Also, the lifestyle interventions that are routinely recommended and shown to be effective are not necessary applicable to this patient population and have not been studied systematically. The threshold for initiating drug therapy is also a matter of debate as discussed subsequently.
Non drug management and prevention
All pregnant women with hypertension are candidates for close supervision and limitation of activities. Bed rest in left lateral position was believed to be useful but is not routinely recommended owing to the socioeconomically factors and the risk of deep vein thrombosis. A nutritious diet rich in calcium should be encouraged in all pregnant women. Calcium supplementation-up to 2g/day may be added since it has shown to reduce the incidence of gestational hypertension and preeclampsia (15, 16). However, salt restriction and weight reduction in obese, a routine practice in non-pregnant women and male hypertensives, is not recommended during pregnancy since it interferes with uteroplacental circulation and fetal growth.
Drug therapy for hypertension
As discussed previously, there is no clear evidence about most drugs regarding their safety, especially to the fetus or efficacy during pregnancy. All drugs should be presumed to cross placenta and affect the fetus. The goal of treatment is to reduce maternal end organ damage and it has been shown that systolic hypertension is more important in this regard in the pregnant hypertensive (17). Centrally acting Methyldopa, calcium antagonist Nifedipine and combined α and β blocker-Labetalol are the most studied and recommended drugs in this situation.
Methyldopa is generally considered the drug of first choice by most clinicians worldwide. It has a long history of safety, proven efficacy and relatively few side effects. It does not interfere with maternal cardiac output and utero-placental circulation and has been used for long durations throughout pregnancy (Table 1). There has been some concern now related to the occurrence of depression in the post partum period hence it is not recommended to be used after the second day of delivery.
Labetalol is fast becoming popular in pregnancy since its efficacy was shown to be similar to methyldopa in a trial comparing these two drugs with each other and to placebo (18). The 2010 NICE guidelines keep it as the drug of first choice while the 2001 American College of Obstetricians and Gynecologists practice bulletin supports Labetalol or methyldopa as the first line agent. It can be given orally as well as intravenoulsly but has the potential to cause fetal growth retardation and neonatal bradycardia.
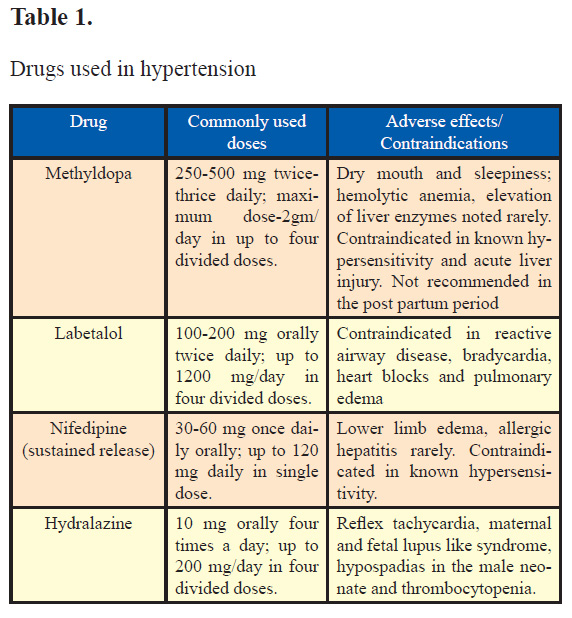
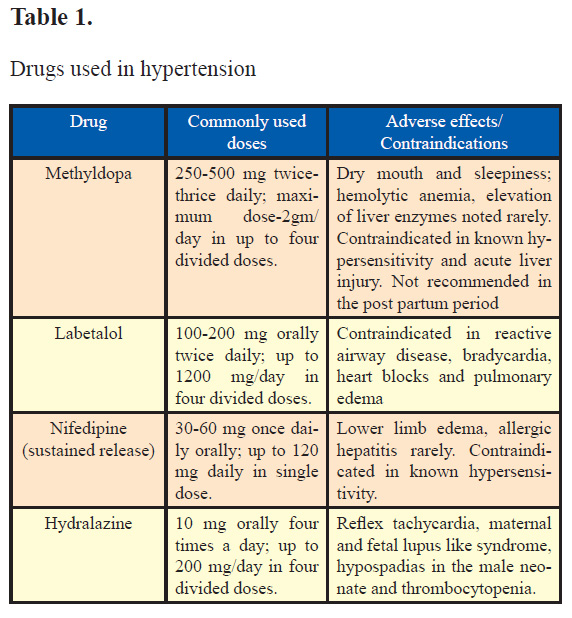
Long acting formulation of oral Nifedipine has been used safely in later half of pregnancy but can cause serious hypotension when used concomitantly with Magnesium Sulphate (used to prevent pre-eclampsia and treat seizures). It also has a tocolytic effect and is generally avoided
Long acting formulation of oral Nifedipine has been used safely in later half of pregnancy but can cause serious hypotension when used concomitantly with Magnesium Sulphate (used to prevent pre-eclampsia and treat seizures). It also has a tocolytic effect and is generally avoided
Angiotensin converting enzyme inhibitors (ACEIs) and angiotensin II receptor blockers are known to be fetotoxic and contraindicated in pregnancy. They are known to cause oligohydramnios, fetal renal dysplasia, anuria and even death. Similarly, diuretics should not be used since they can compromise on intravascular fluid volume and uteroplacental circulation. Atenolol is also to be avoided since it interferes with fetal growth.
The ongoing treatment for hypertension may be required to be continued in the post partum period, especially for women with chronic hypertension. In women who did not have hypertension before pregnancy, or with unknown pre-pregnancy status, one may stop treatment after 3-4 weeks and assess the need by measuring BP at weekly intervals for a month and then at monthly intervals for a year. If the BP rises again, it should be treated accordingly.
There has been considerable controversy and debate regarding the treatment threshold for hypertension in pregnancy in the absence of pre-eclamptic features. The general consensus now emerging is that mild to moderate BP elevation has no harmful effects on the mother or the fetus (20). On the contrary, attempts at lowering the BP in this range may result in placental hypo perfusion resulting in growth retardation. It also does not prevent the occurrence of preeclampsia. Therefore, it is now generally accepted that BP in the range of 150-160 mmHg systolic and/or 100-110 mmHg diastolic should be treated to minimize maternal risk.
Hypertensive emergency during pregnancy
It is defined as presence of severely increased blood pressure or evidence of maternal and fetal compromise. Immediate hospitalization is required in this situation along with the use of drugs with rapid onset of action. The systolic blood pressure should be lowered by about 25% over a period of few hours. Intravenous Labetalol, Hydralazine, Sodium Nitroprusside or Nitroglycerine and oral Nifedipine and Methyldopa are the drugs available for this situation. Labetalol is the drug of choice these days since it is safe, rapid acting and does not cause cerebral edema. It is however contraindicated in presence of heart blocks, heart failure, bronchial asthma and can cause fetal bradycardia. Intravenous Hydralazine and sodium Nitroprusside are no longer considered safe for use in pregnancy due to the risk of adverse perinatal events (Hydralazine) and fetal cyanide poisoning (Nitroprusside) (21).
Rapid acting oral Nifedipine is also not recommended since it can cause severe hypotension and cerebral infarction. Intravenous nitroglycerine is a good option in the situation of pulmonary edema (5μg/min -100μg/min titrated every 3-5 minutes). Close hemodynamic monitoring is recommended with the use of nitroglycerine to tailor the therapy according to the blood pressure.
Management of Preeclampsia/Eclampsia
The management of preeclampsia encompasses much more than BP control alone.
Close coordinated approach of the Obstetrician, Gynecologist and treating physician is necessary to ensure safety of mother and fetal well-being.
Prevention
The first step is prevention of development of preeclampsia altogether in high risk women. Aspirin is the drug of choice and is recommended in doses of 75-100 mg daily in women with high-risk maternal histories (22). Calcium supplementation has also been found useful in women who have a high risk of preeclampsia with low intake of calcium. Multivitamin and mineral supplements, low salt diet or folic acid are not beneficial and are thus not recommended in his situation. Ergometrine and Oxytocin, often used as a combination to precipitate delivery of placenta and prevent post partum hemorrhage, should not be used in pregnant women with hypertension. Ergometrine is a powerful vasoconstrictor and can precipitate hypertension, as such; Oxytocin alone may be used in this situation. Similarly, there is no role for intravenous fluids or diuretics routinely in case of oliguria, a finding in patients with preeclampsia.
The drug of choice for prevention of seizures in preeclampsia is intravenous Magnesium sulphate (23). It is given as 4-6 gm diluted in 100 ml saline, infused over 15-20 minutes. This is followed by an infusion of 2 gm per hour continued for up to 12-24 hours post partum. Caution should be exercised in patients with renal impairment and a therapeutic serum level of 4-7mg/dl should be maintained. Magnesium Sulphate has been found useful in treatment of seizures too and is considered superior for prevention of recurrence of seizures as compared to Phenytoin.
Definitive treatment of preeclampsia/eclampsia is delivery of the fetus. It significantly reduces the risk of seizures, pulmonary edema, abruptio placenta, disseminated intravascular coagulopathy and cerebral edema but may not be the best option for the fetus, specially in the early stages of gestation. Therefore, judicious management of the situation with close monitoring of mother and fetus is essential. The decision to deliver the fetus should be only be taken after taking into account the gestational age, maternal risk, fetal distress etc. The detailed management of preeclampsia/eclampsia is beyond the scope of current discussion and is not discussed here.
BP management Postpartum
As discussed earlier, BP usually rises in the first few days after delivery before normalizing. Close monitoring and follow up is required during this period in hypertensive mothers. All the drugs are excreted in the breast milk and caution should be exercised in choosing the drugs. The same drugs used in pregnancy may be continued postpartum also since there is no long term data for the effect on the lactating child. It should be remembered that Bromocriptine, sometimes used for suppression of lactation, causes elevation of BP and methyldopa, considered safe during pregnancy has shown to increase post partum depression. Labetalol, Nifedipine and Metoprolol have been shown to have no effect on the fetus and may be safely used. Even Enalapril and Captopril have been shown to be safe during this period (24).
Long term implications
Women who develop hypertension during pregnancy are at risk of developing hypertension in future pregnancies. The earlier the onset of hypertension in the first gestation, the higher is the risk in subsequent pregnancies.
Similarly women developing hypertension and preeclampsia are at increased risk of cerebrovascular events and coronary artery disease later in the life (25, 26).
Summary
Hypertension during pregnancy is common and it complicates around 5-10% of all pregnancies. It is a unique subset of hypertension requiring thorough understanding of the physiology and deep insights into the various aspects of its diagnosis and management by the obstetrician/gynecologist and cardiologists. The precise cutoffs for treatment have not been defined but it is generally agreed that mild to moderate elevations in BP need not be treated in pregnancy as it can interfere with placental perfusion and fetal well being. Also, there is a paucity of good quality data regarding the optimal antihypertensive drugs in pregnancy and the most common drugs used in nonpregnant adults, like ACEIs and angiotensin receptor blockers are contraindicated in pregnancy. Methyldopa and Labetalol are currently being the drugs of choice for hypertension in pregnancy.
Preeclampsia/eclampsia is a devastating complication of hypertension in pregnancy and should be suspected, prevented and judiciously managed.
References
- Roberts JM, Pearson G, Cutler J, Lindheimer M. Summary of the NHLBI working group on research on hypertension during pregnancy. Hypertension. 2003;41:437-45.
- Centre for Maternal and Child Enquiries (CMACE). Saving mothers’ lives: reviewing maternal deaths to make childhood safer: 2006-08.The Eighth report on confidential enquiries into maternal deaths in the United Kingdom. BJOG. 2011;118(Suppl1):1-203.
- Report of the national high blood pressure education programme working group on high blood pressure in pregnancy. Am J Obstet Gynecol. 2000;183:S1-S22.
- Clapp JF III, Capeless E. Cardiovascular function before, during and after the first and subsequent pregnancies. Am J Cardiol. 1997;80:1469-73.
- European Society of Hypertension-European Society of Cardiology Guidelines Committee. 2003 European Society of Hypertension-European Society of Cardiology guidelines for the management of arterial hypertension. J Hypertens. 2003;21:1011-53.
- Walker SP, Higgins JR, Brennecke SP. The diastolic debate; is it time to discard Korotkoff phase IV in favor of V for blood pressure measurements in pregnancy? Med J Aust. 1998;169:203-5.
- Penny JA, Halligan AWE, Shennan AH, Lambert PC, Jones DR, de Swiet M. Automated, ambulatory or conventional BP measurement in pregnancy: which is better predictor of severe hypertension? Am J Obstet Gynecol. 1998;178:521-6.
- Staessen JA, Asmar R, De Buyzere M, Imai Y, Parati G, Shimada K, Stergiou G, Redón J, Verdecchia P; Participants of the 2001 Consensus Conference on Ambulatory Blood Pressure Monitoring. Blood pressure measurement and cardiovascular outcome. Blood Press Monit. 2001;6:355-70.
- Levine RJ, Ewell MG, Hauth JC, Curet LB, Catalano PM, Morris CD, Choudhary G, Sibai BM. Should the definition of pre-eclampsia include a rise in blood pressure of > 90 mmHg in association with proteinuria? Am J Obstet Gynecol. 2000;183:787-92.
- ESC guidelines on the management of cardiovascular diseases during pregnancy of the European society of Cardiology (ESC). Eur Heart J. 2011;32:3147-97.
- Hiett AK, Brown HL, Britton KA. Outcome of infants delivered between 24 and 28 weeks’ gestation in women with severe pre-eclampsia. J Matern Fetal Med. 2001;10:301-4.
- Roberts JM, Pearson G, Cutler J, Lindheimer M. Summary of the NHLBI Working Group on research on hypertension during pregnancy. Hypertension. 2003;41:437-45.
- Rossi GP, Seccia TM, Pessina AC. Clinical use of laboratory tests for the identification of secondary forms of arterial hypertension. Crit Rev Clin Lab Sci. 2007;44:1-85.
- Redman CW. Fetal outcome in trial of antihypertensive treatment in pregnancy. Lancet. 1976;2:753-6.
- Atallah AN, Hofmeyr GJ, Duley L. Calcium supplementation during pregnancy for preventing hypertensive disorders and related problems (Cochrane Review) in: The Cochrane library, Issue 1. Oxford Update Software, 2000.
- Hofmeyr GJ, Atallah AN, Duley L. Calcium supplementation during pregnancy for preventing hypertensive disorders and related problems. Cochrane Database Syst Rev. 2006; (3):CD001059.
- Martin JN Jr, Thigpen BD, Moore RC, Rose CH, Cushman J, May W. Stroke and severe preeclampsia and eclampsia: a paradigm shift focusing on systolic blood pressure. Obstet Gynaecol 2005;105:246-54.
- Sibai BM, Mabie WC, Shamsa F, Villar MA, Anderson GD. A comparison of no medication versus methyldopa or labetalol in chronic hypertension during pregnancy. Am J Obstet Gynaecol. 1990;162:960-7.
- Khedun SM, Maharaj B, Moodley J. Effects of antihypertensive drugs on the unborn child. What is known, and how should this influence prescribing? Paediatr Drugs. 2000;2:419-36.
- Abalos E, Dudley L Steyn DW, et al. Antihypertensive therapy for mild to moderate hypertension during pregnancy. Cochrane Database Syst Rev. 2007;1:CD002252
- Coppage KH, Sibai BM. Treatment of hypertensive complications in pregnancy. Curr Pharm Des. 2005;11:749-59.
- Dudley L, Henderson-Smart D, Meher S, et al. Antiplatelet agents for preventing pre-eclampsia and its complications. Cochrane Database Syst Rev. 2007;2:CD004659.
- The Magpie Trial Collaborative Group. Do women with pre-eclampsia, and their babies, benefit from magnesium sulphate? The Magpie Trial; a randomized placebo controlled trial. Lancet. 2002;359:1877-90.
- National collaborating centre for women’s and children’s health. Hypertension in pregnancy. The management of hypertensive disorders during pregnancy. London: National Institute of health and Clinical Excellence (NICE); 2010.p.46.(Clinical guideline; no.107).
- Wilson BJ, Watson MS, Prescott GJ, Sunderland S, Campbell DM, Hannaford P, Smith WC. Hypertensive diseases of pregnancy and risk of hypertension and stroke in later life: results from cohort study. BMJ 2003;326:845-51.
- Jonsdottir LS, Arngrimsson R, Geirsson RT, Sigvaldason H, Sigfusson N. Death rates from ischemic heart disease in women with a history of hypertension in pregnancy. Acta Obstet Gynaecol Scand. 1995;74:772-6.
- Why Publish with JCPC?
- Instructions to the Authors
- Submit Manuscript
- Advertise with Us
- Journal Scientific Committee
- Editorial Policy
Print: ISSN: 2250-3528


