The Journal of Clinical and Preventive Cardiology has moved to a new website. You are currently visiting the old
website of the journal. To access the latest content, please visit www.jcpconline.org.
Case Report
Echocardiographic Diagnosis of Ruptured Sinus of Valsalva with Congenital VSD and AR
Volume 4, Jan 2015
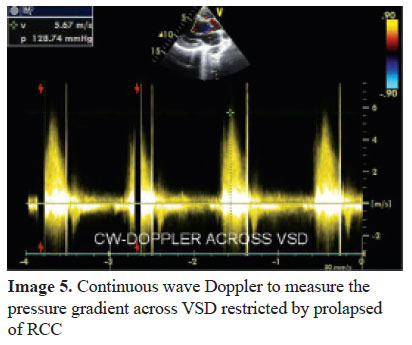
Sitaram Gupta, MBBS, MD, PGDCC, Ram Chitlangia, MBBS, MD, DM, Deepak Garg, MBBS, PGDCC, Jaipur, India
J Clin Prev Cardiol. 2015;4(1):24-6
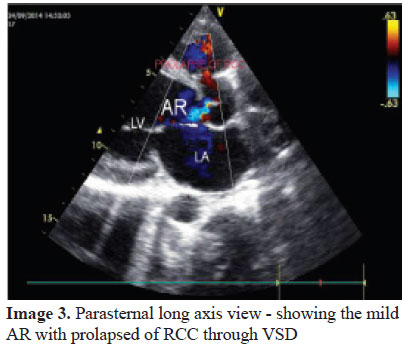
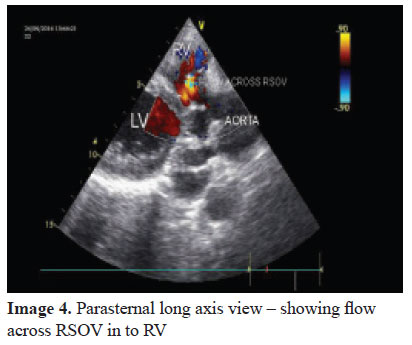
Rupture of Sinus of Valsalva is rare but potentially life threatening clinical entity which requires immediate recognition and intervention. The presentation may range from an asymptomatic continuous murmur to acute cardiogenic shock and death. RSOV is either isolated lesion or associated with ventricular septal defect (VSD). Defect in this part of the ventricular septum involve the infundibular septum and thus lie underneath both semilunar valves. Lack of supporting tissue for the aortic annulus precipitate prolapse of aortic cusp in to RV and aneurysm of sinus of Valsalva. This aneurysm has potential to get ruptured (1). Most of the times, the VSDs associated with RCC prolapse with RSOV are doubly committed VSDs.Echocardiography has become the definitive investigation tool not only to define and diagnose the lesion but also to quantify its severity. Thus it plays a critical role in management of the patient (2).
Case Report
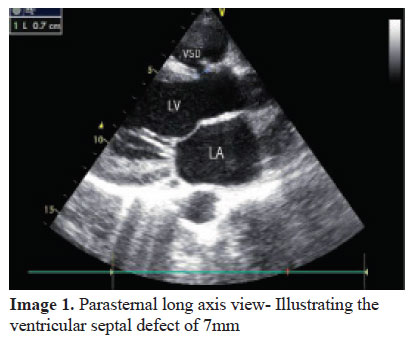
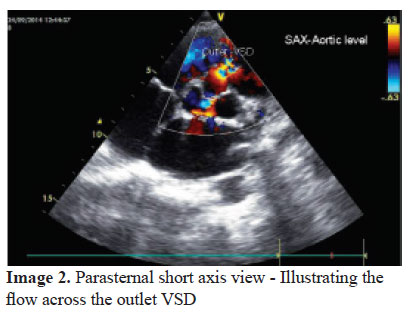
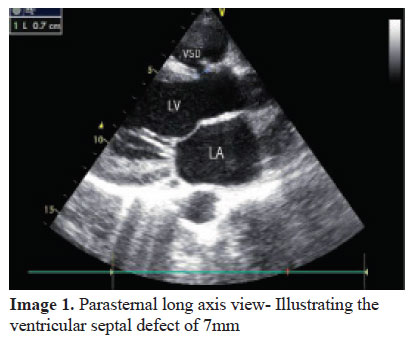
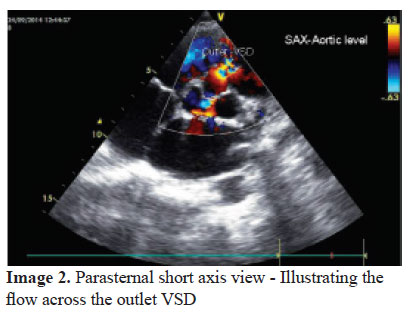
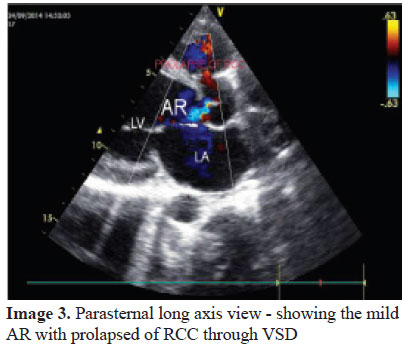
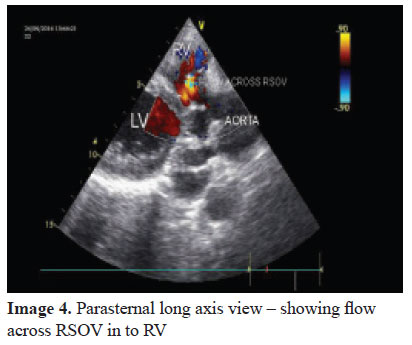
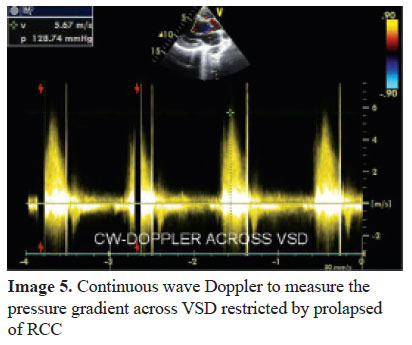
A 27-year-old male with a history of childhood murmur was a diagnosed case of VSD. This person was referred ABSTRACTto our institution for progressive heart failure symptoms with pricking chest pain especially on bending forward for last one year. On physical examination he had BP of 120/50 mmHg and pulse was 80/min. On cardiac examination systolic thrill and continuous murmur over the left sternal border was detected. Electrocardiogram was normal. A chest radiograph demonstrated a slightly enlarged cardiac silhouette and increased pulmonary blood flow. Transthoracic echocardiography demonstrated normal LV systolic functions. There was sub aortic VSD of around 7 mm below the aortic valve and discontinuity in the wall of right coronary sinus. Color flow Doppler revealed a continuous turbulent flow between right sinus of Valsalva and the right ventricle (above the aortic valve). Prolapse of RCC (which is restricting the VSD) in to RV with mild eccentric AR was also noticed. The diagnosis was confirmed in operating room and patient underwent successful patch closure of the VSD along with repair of the RSOV. The dyspnea improved postoperatively and the patient is doing fine on follow-up
Discussion
Ruptured sinus of Valsalva is an uncommon condition with protean clinical manifestation. Rupture is often with an abrupt onset and the presentation may range from an asymptomatic murmur to acute cardiogenic shock and death.
A retrospective analysis of RSOV cases reported in Singapore General Hospital revealed that half of the cases were having VSD and 1/3rd cases were associated with AR. Rupture of right coronary cusps was much more common (83%) than non-coronary cusp (17%) and left coronary cusp (0%). Most of the RCC ruptures were directed into the RV and all of the NCC ruptures were into the RA (3).
Males are more affected than females (3:1 ratio), and the prevalence is higher in the Eastern than in the Western population (4).
Transthoracic echocardiography is the main diagnostic tool for the identification of the RSOV, while transesophageal imaging may further help the diagnosis and in surgical correction of the lesion, especially when VSD is also present. Echocardiography can also provide important information necessary for the differential diagnosis from other disorders which cause continuous murmur, such as patent ductus arteriosus, aorticopulmonary window, coronary fistula, as well as co-existing VSD and aortic valve regurgitation (5).
In conclusion, RSOV is a rare condition with a varied presentation that sometimes can be fatal if not diagnosed quickly. Right coronary sinus of Valsalva to right ventricle ruptures are the commonest type of RSOV and there is an association with VSD, aortic regurgitation and infective endocarditis. Trans-thoracic echocardiography is the reliable diagnostic tool for the identification of the aneurysms of sinus of Valsalva, while multiplane trans-esophageal imaging may further help in the diagnosis and intraoperative surgical correction of the lesion, especially when VSD is also present.
References
- AR Moarref, S Afifi, M Jannati, GR Rezaian. Ruptured sinus of valsalva aneurysm initially misdiagnosed as ventricular septal defect by echocardiography. Iranian Cardiovascular Research Journal 2009;3:123-5.
- Grosz C, Pais R, Poanta L.. Rupture sinus of Valsalva in a patient with dextrocardia. Case report. Med Ultrason. 2011;13:323-5.
- Shah RP, Ding ZP, Ng AS, Quek SS.. A ten –year review of ruptured sinus of valsalva: Clinico-Pathological and ECHO-Doppler Features. Singapore Med J 2001;42:473-6.
- Tipoo Sultan FA, Basir N, Fatimi S. Aneurysm of Sinus of Valsalva. J Coll Physicians Surg Pak. 2011;21:173-5.
- Lakoumentas JA, Bonou MS, Brili S, Theocharis CS, Benroubis AD, Perpinia AS, Harbis PK. Ruptured Aneurysm of the Right Sinus of Valsalva Into the Right Ventricle. Hellenic J Cardiol. 2002;43:242-5.
- Why Publish with JCPC?
- Instructions to the Authors
- Submit Manuscript
- Advertise with Us
- Journal Scientific Committee
- Editorial Policy
Print: ISSN: 2250-3528


