The Journal of Clinical and Preventive Cardiology has moved to a new website. You are currently visiting the old
website of the journal. To access the latest content, please visit www.jcpconline.org.
Images in Cardiology
Communication Between Distal Ascending Aorta and Adjacent Superior Vena cava
Volume 2, Apr 2013
Sita Ram Mittal, MD, DM, Ajmer, India
J Clin Prev Cardiol 2013;2(2):106-7
A two months old child was refered for echocardiography for tachypnea. Echocardiography revealed mid systolic reduction in pulmonary artery flow (Figure 1A), severe pulmonary artery hypertension (right ventricular systolic pressure of 89.3 mmHg calculated from tricuspid regurgitation jet), dilated right atrium and right ventricle and a small (4.5 mm) ostium secundum atrial septal defect with right to left shunt (Figure 1B). Supra sternal view with colour Doppler revealed a turbulent jet in superior vena cava which was arising from distal ascending aorta near the beginning of aortic arch (Figure 1C). Pulsed wave Doppler confirmed continuous flow between aorta and superior vena cava (Figure 1D). Parents did not agree for CT angio or catheterization.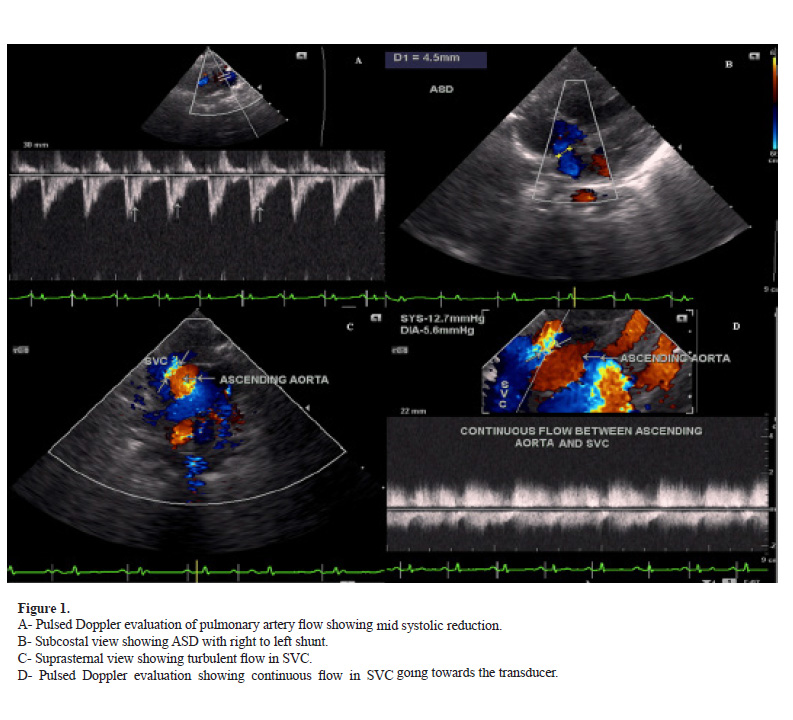
Common causes of shunt between aorta and venous side of circulation are ruptured sinus of valsalva and coronary arterio-venous fistula. Uncommon causes include congenital tunnel between aorta & right sided chambers or rupture of a dissecting aneurysm of ascending aorta. These lesions commonly drain into right atrium, right ventricle or pulmonary artery. Communication with superior vena cava are rare. When present, such communications are confined to proximal part of SVC close to its junction with right atrium.
Theron et al. (1) have reported a case of traumatic aortovena caval fistula. Toyoda et al. have reported rupture of a dissecting aneurysm into superior vena cava in a case of Marfan’s syndrome (2). Oomman et al. have reported a case of congenital aortocaval fistula between right aortic sinus and superior vena cava just above SVCright atrial junction (3).
Our case is different from these cases. In our case, aortocaval communication was between distal ascending aorta and adjacent superior vena cava. In view of the age of the patient and the absence of any other apparent factor, our case was probably congenital in origin. The child did not have any lung parenchymal disease. Elevated pulmonary artery pressure was an isolated association probably because of persistent pulmonary arterial hypertension.
Source of Funding
None
Conflict of Interest
None
References
- Theron HD, Otto AC, Van Aswengen A, Herbst CP, Kleijnhans PH, Lotter MG et al. Traumatic aorto-vena caval fistula detected with radionuclide angiocardiography. A case report. S Afr Med J. 1985;28:489-90.
- Toyoda Y, Yamashita C, Yoshida M, Nohara H, Okada K, Otaki Y, Okada M. Rupture of a dissecting aneurysm into the superior vena cava in Marfan’s syndrome. J Cardiovasc Surg (Torino). 1997;38:411-3.
- Oomman A, Mao R, Krishnan P, Girinath MR. Congenital aorto-vena caval fistula to the superior vena cava. Ann Thorac Surg. 2001;72:911.
- Why Publish with JCPC?
- Instructions to the Authors
- Submit Manuscript
- Advertise with Us
- Journal Scientific Committee
- Editorial Policy
Print: ISSN: 2250-3528


