The Journal of Clinical and Preventive Cardiology has moved to a new website. You are currently visiting the old
website of the journal. To access the latest content, please visit www.jcpconline.org.
Review Article
Cardiorenal Syndromes
Volume 1, Oct 2012
Shyam Bansal, MD, DM, Vijay Kher, MD, DM, Gurgaon, India
J Clin Prev Cardiol 2012;1(4):174-84
Cardiovascular diseases are the commonest cause of morbidity and mortality worldwide. In USA, about one third of population has some form of cardiovascular disease, i.e., hypertension, coronary heart disease (CHD), heart failure (HF), stroke, peripheral vascular disease (PVD) (1). Chronic kidney disease (CKD) affects about 13% of population in USA (2). There is a close relationship between cardiac and kidney diseases, as patients with cardiac disease often develop kidney dysfunction and the most common cause of mortality in patients with kidney disease is cardiovascular (3). Patients with CKD have 10–20 times high chances of cardiovascular disease as compared to age-matched non-CKD population (4). Similarly patients with acute cardiac dysfunction like acute HF or acute coronary syndrome (ACS) may develop acute kidney injury (AKI) and vice versa (5). However, despite this knowledge, the relationship between cardiac and kidney diseases has not been well defined till now, resulting in difficulty in managing these patients. The term cardiorenal syndrome (CRS) is used to define this heart and kidney interaction, and has been in use for sometime now, but a proper identification and classification system was lacking (6). Recently in 2008, the acute dialysis quality initiative (ADQI) group organized a consensus conference in Venice, Italy to discuss this issue, comprising of opinion leaders and experts from nephrology, critical care, cardiology, cardiac surgery and epidemiology (7). The group came out with consensus definition and classification of CRSs.The following definitions were proposed:
Term CRS was defined as disorder of heart or kidneys, whereby acute or chronic dysfunction in one organ may induce acute or chronic dysfunction of the other organ (8).
Five subtypes of CRS were defined as follows:
Five subtypes of CRS were defined as follows:
- Acute CRS (Type 1) – an acute worsening of cardiac function leading to renal dysfunction
- Chronic CRS (Type 2) – chronic abnormality of cardiac function leading to renal dysfunction
- Acute renocardiac syndrome (Type 3) – acute worsening of renal function, leading to cardiac dysfunction
- Chronic renocardiac syndrome (Type 4) – chronic abnormality of renal function, leading to cardiac dysfunction
- Secondary CRSs (Type 5) – systemic conditions leading to both cardiac and renal dysfunction; these include amyloidosis, diabetes mellitus, sepsis and systemic lupus erythematous (SLE), etc.
The ADQI group recognized that many patients might migrate to different groups during the course of their illness and so the classification is not fixed.
Acute cardiorenal syndrome (Type 1)
This is a condition characterized by acute worsening of heart function, i.e., acute decompensated heart failure (ADHF), ACS and cardiac surgery associated low cardiac output, which leads to AKI (9).
Many studies have used the term worsening renal failure (WRF) to define AKI and the incidence of WRF in patients with ADHF and ACS is found to be between 24–45% and 9–19%, respectively. This wide range in incidence is due to different definitions of WRF and heterogeneity of these studies (10-13). Various studies have defined various levels of rise in serum creatinine as criteria of renal dysfunction, from increase of 0.3 mg or 0.5 mg to >25% decrease in glomerular filtration rate (GFR) (10–15). Newly validated Risk, Injury, Failure, Loss, ESKD (RIFLE) and Acute Kidney Injury Network (AKIN) criteria for AKI take into account a rise in creatinine of >0.3 mg/dL or >25% decrease in GFR, apart from decrease in urine output of <0.5 mL/kg/h for 6 h (16).
Most of this kidney dysfunction due to ADHF/ACS occurs early after admission; however, it can occur any time after hospitalization. The ADQI suggests that AKI associated with ADHF/ACS should be considered within 1 week of hospitalizations, as >90% of patients develop AKI within this duration (17). Patients admitted with ACS/ADHF who develop AKI have higher chances of all cause and cardiovascular mortality, prolonged hospitalization, recurrent admissions and higher chances of progression to advanced CKD stages (12–15).
The acute decompensated heart failure national registry (ADHERE) examined >105,000 patients with ADHF and found that preexisting renal insufficiency was present in 30% of cases and 21% had serum creatinine levels >2 mg/dL. The study also found that the best single predictor of inpatient mortality was high levels of blood urea nitrogen and serum creatinine levels (>43 and 2.75 mg/dL, respectively) at admission (18).
Chronic cardiorenal syndrome (Type 2)
Chronic CRS is defined as chronic cardiac abnormality leading to CKD. The chronic cardiac abnormalities include congenital heart diseases (CHD), chronic HF, atrial fibrillation, constrictive pericarditis and chronic ischemic heart diseases (17). Sometimes preexisting CKD is present and it is not always possible to distinguish between type 2 and type 4 CRS (9). The prevalence of kidney dysfunction in patients with chronic cardiac diseases is estimated between 45% and 63% in various studies. There is higher morbidity and mortality in patients with CHF and CKD as compared to patients without kidney disease (19–23).
One of the typical examples of type 2 CRS is CHD, in which long-standing cardiac disease results in alteration in renal perfusion and neurohormonal activation resulting in CKD. In a study of 1102 patients with CHD, over 50% had evidence of kidney dysfunction and 9% had GFR <60 mL/min, and these patients had three-fold higher mortality as compared to other patients (23).
Another evidence of type 2 CRS is provided by Atheroscerosis Risk in Community and Cardiovascular Health (24). In this study, 12.9% of study population had cardiovascular disease at baseline. These patients had a mean baseline serum creatinine of 0.9 mg/dL and estimated glomerular filtration rate (eGFR) 86.2 mL/min/1.73 m2. After a mean follow-up of 9.3 years, 7.2% of CVD patients had reduced kidney function when defined as a serum creatinine increase of ≥0.4 mg/dL and 34% when defined as a decrease in eGFR >15 mL/min/1.73 m2. During the observational period, 2.3% and 5.6% developed new kidney disease, respectively. By multivariable analysis, baseline CVD was independently associated with both decline in kidney function and development of new CKD.
One of the typical examples of type 2 CRS is CHD, in which long-standing cardiac disease results in alteration in renal perfusion and neurohormonal activation resulting in CKD. In a study of 1102 patients with CHD, over 50% had evidence of kidney dysfunction and 9% had GFR <60 mL/min, and these patients had three-fold higher mortality as compared to other patients (23).
Another evidence of type 2 CRS is provided by Atheroscerosis Risk in Community and Cardiovascular Health (24). In this study, 12.9% of study population had cardiovascular disease at baseline. These patients had a mean baseline serum creatinine of 0.9 mg/dL and estimated glomerular filtration rate (eGFR) 86.2 mL/min/1.73 m2. After a mean follow-up of 9.3 years, 7.2% of CVD patients had reduced kidney function when defined as a serum creatinine increase of ≥0.4 mg/dL and 34% when defined as a decrease in eGFR >15 mL/min/1.73 m2. During the observational period, 2.3% and 5.6% developed new kidney disease, respectively. By multivariable analysis, baseline CVD was independently associated with both decline in kidney function and development of new CKD.
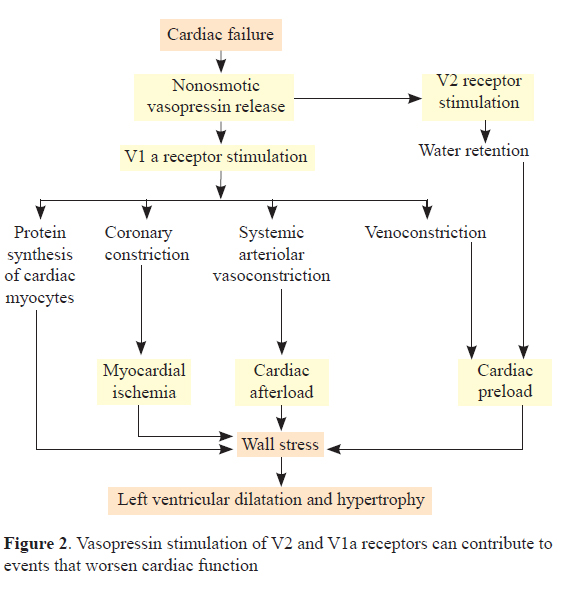
Pathophysiology of cardiorenal syndrome (Figures 1 and 2)
The exact mechanism of renal dysfunction in HF is not well-understood. The most common explanation has been that decrease in cardiac output as a result of poor cardiac function results in reduced renal perfusion leading to kidney dysfunction (25–27).
Poor perfusion to kidneys leads to activation of neurohormonal system, resulting in activation of arterial baroreceptors and intrarenal sensors. These lead to activation of renin angiotensin aldosterone system (RAAS), sympathetic nervous system and also arginine vasopressin system. The activation of RAAS results in increase in angiotensin II and aldosterone; the binding of angiotensin II to AT1 receptor leads to vasoconstriction and aldosterone secretion. Aldosterone promotes reabsorption of sodium in distal tubules leading to water and salt retention and worsening of pulmonary vascular congestion. Another mediator which is increased in this condition is endothelin I, which leads to afferent arteriolar constriction, further reducing the renal perfusion and exacerbating renal injury. Blockage of endothelin receptors in animal models has shown to improve GFR and blood flow (26).
In addition to the above effects, RAAS activation causes activation of NADPH oxidase, which results in the formation of reactive oxygen species (ROS); this increase in oxidative stress leads to production of proinflammatory cytokines, like interleukin-1, interleukin-6, C-reactive protein (CRP) and tumor necrosis factor (TNF). These cytokines have negative inotropic effects, assist in cardiac remodeling and cause thrombotic complications (27). Arginine vasopressin (AVP) causes fluid retention and enhances actions of angiotensin II and norepinephrine.
However, recent data suggests that there may be other mechanisms of CRS. Evaluation Study of Congestive heart failure And Pulmonary artery catheterization Effectiveness (ESCAPE) randomized 433 HF patients to receive therapy guided by pulmonary artery catheterization or by clinical assessment alone (28). The result in 193 patients treated with pulmonary catheter showed that there was no correlation between serum creatinine or GFR and pulmonary capillary pressure, cardiac index or systemic vascular resistance. And even increasing their cardiac index (1.9–2.4 mL/m2) did not improve the renal dysfunction. A significant correlation between right atrial pressure with serum creatinine or GFR was observed, suggesting a role of high central venous pressure in renal dysfunction. In a study of 145 patients with HF, patients with higher central venous pressure had higher risk of renal function deterioration and a reduction in central venous pressure to <8 cm resulted in improvement in renal function (29). The change in cardiac index did not change GFR during hospitalization. This is explained by high venous pressure which leads to reduction in perfusion pressure across glomeruli resulting in reduction in GFR (29,30).

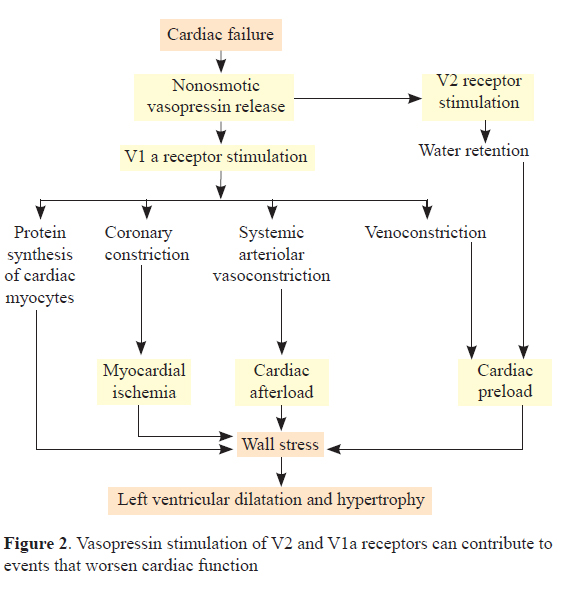
Poor perfusion to kidneys leads to activation of neurohormonal system, resulting in activation of arterial baroreceptors and intrarenal sensors. These lead to activation of renin angiotensin aldosterone system (RAAS), sympathetic nervous system and also arginine vasopressin system. The activation of RAAS results in increase in angiotensin II and aldosterone; the binding of angiotensin II to AT1 receptor leads to vasoconstriction and aldosterone secretion. Aldosterone promotes reabsorption of sodium in distal tubules leading to water and salt retention and worsening of pulmonary vascular congestion. Another mediator which is increased in this condition is endothelin I, which leads to afferent arteriolar constriction, further reducing the renal perfusion and exacerbating renal injury. Blockage of endothelin receptors in animal models has shown to improve GFR and blood flow (26).
In addition to the above effects, RAAS activation causes activation of NADPH oxidase, which results in the formation of reactive oxygen species (ROS); this increase in oxidative stress leads to production of proinflammatory cytokines, like interleukin-1, interleukin-6, C-reactive protein (CRP) and tumor necrosis factor (TNF). These cytokines have negative inotropic effects, assist in cardiac remodeling and cause thrombotic complications (27). Arginine vasopressin (AVP) causes fluid retention and enhances actions of angiotensin II and norepinephrine.
However, recent data suggests that there may be other mechanisms of CRS. Evaluation Study of Congestive heart failure And Pulmonary artery catheterization Effectiveness (ESCAPE) randomized 433 HF patients to receive therapy guided by pulmonary artery catheterization or by clinical assessment alone (28). The result in 193 patients treated with pulmonary catheter showed that there was no correlation between serum creatinine or GFR and pulmonary capillary pressure, cardiac index or systemic vascular resistance. And even increasing their cardiac index (1.9–2.4 mL/m2) did not improve the renal dysfunction. A significant correlation between right atrial pressure with serum creatinine or GFR was observed, suggesting a role of high central venous pressure in renal dysfunction. In a study of 145 patients with HF, patients with higher central venous pressure had higher risk of renal function deterioration and a reduction in central venous pressure to <8 cm resulted in improvement in renal function (29). The change in cardiac index did not change GFR during hospitalization. This is explained by high venous pressure which leads to reduction in perfusion pressure across glomeruli resulting in reduction in GFR (29,30).

Acute renocardiac syndrome (Type 3)
Acute renocardiac syndrome is seen in patients with AKI, which can lead to acute cardiac dysfunction, for example, ACS or cardiac arrhythmia. This is supposed to be caused by accumulation of uremic toxins, fluid and salt retention, accelerated hypertension and electrolyte disturbances, etc. Various diseases incriminated are postinfectious glomerulonephritis, rhabdomyolysis, and drug-induced AKI. AKI after contrast agents or cardiac surgery can also lead to cardiac dysfunction and included in type 3 CRS (9,17). Contrast nephropathy is common after use of contrast agents, and most patients recover renal functions; however, a small percentage of these patients (0.2–1.1%) do not recover kidney function and require long-term renal replacement therapy and these patients can develop secondary cardiac dysfunction due to renal failure (31,32). The risk factors are older age, preexisting CKD, DM, CAD, PVD and higher volume of contrast medium. However, the exact incidence and epidemiology of this syndrome is not clear because of different definitions used and variable risk factors (17).
Chronic renocardiac syndrome (Type 4)
Cardiovascular diseases are the leading cause of death in patients with CKD. CKD can cause either reduction in cardiac function (left ventricular hypertrophy or diastolic dysfunction) or cardiovascular disease (HF, MI or stroke) (9,17). Several studies have demonstrated that the risk of CVD mortality is 10–20 times higher in CKD patients as compared to age- and sex-matched population. About 50% of patients of CKD die of cardiovascular diseases (3,4). The risk of CVD increases as the grade of CKD increases and risk is highest in patients on dialysis (33,34). Both traditional risk factors like presence of diabetes, hypertension, increased age, dyslipidemia, etc. and nontraditional risk factors related to uremia, for example, abnormities in calcium phosphorus metabolism, chronic inflammation, endothelial dysfunction, vascular remodeling, and oxidative stress, etc. are responsible for this increased risk (33–35). Secondary cardiorenal syndromes (Type 5)
Many systemic diseases can lead to simultaneous involvement of heart and kidney. The exact epidemiology of this syndrome is not known because of different diseases causing it. There is incomplete understanding of pathophysiological mechanism causing this syndrome, whether it is truly bidirectional or concurrent involvement of both organs. The prototype diseases are diabetes, amyloidosis, sepsis, SLE etc. (17).
Sepsis is a common condition which can frequently lead to simultaneous AKI and cardiac dysfunction. Approximately, 11–64% of patients with sepsis develop AKI (36,37). Numerous studies have shown that morbidity and mortality is much higher in patients with sepsis and AKI as compared with sepsis or AKI alone (38,39). Similarly, cardiac dysfunction is very common in patients with sepsis and up to 30–80% of patients with sepsis have elevated cardiac troponin levels and it correlates with reduced left ventricular function (40,41). The mortality in these patients is very high. However, there is a lack of studies that have specifically examined the incidence, risk factors, pathophysiology and outcomes of this syndrome.
Sepsis is a common condition which can frequently lead to simultaneous AKI and cardiac dysfunction. Approximately, 11–64% of patients with sepsis develop AKI (36,37). Numerous studies have shown that morbidity and mortality is much higher in patients with sepsis and AKI as compared with sepsis or AKI alone (38,39). Similarly, cardiac dysfunction is very common in patients with sepsis and up to 30–80% of patients with sepsis have elevated cardiac troponin levels and it correlates with reduced left ventricular function (40,41). The mortality in these patients is very high. However, there is a lack of studies that have specifically examined the incidence, risk factors, pathophysiology and outcomes of this syndrome.
Diagnosis and Biomarkers of Cardiorenal Syndromes
Biomarkers in cardiorenal syndrome
Biomarkers are routinely used for early diagnosis in patients with ACS or HF, and they have been found to be useful in these conditions. Recently various biomarkers have been proposed for early diagnosis in patients with AKI, especially after CABG; however, they are still not used widely. Some of these biomarkers were proposed for diagnosis of AKI in patients with CRSs during the recent ADQI meeting (7).
Biomarkers of heart failure
Natriuretic peptide
B-type natriuretic peptides (NT pro-BNP and BNP) are elevated in patients with ADHF and they are established diagnostic tools. High levels of these peptides are also seen in patients with ACS, stable HF and associated with increased cardiovascular events and mortality in these patients (42,43). Natriuretic peptides are increased in patients with type 1 HRS and can be used as a marker. Patients with CKD have high levels of natriuretic peptides as compared to patients with normal kidney function even in the absence of CHF. However, BNP has been shown to have prognostics utility in patients with various stages of CKD, demonstrating prognostic utility in CRS type 2 and type 4 (44, 45).
Neutrophil gelatinase associated lipogalin (NGAL)
Biomarkers of renal injury
Neutrophil gelatinase associated lipogalin (NGAL)
NGAL is a protein, expressed at low levels by various human tissues, including kidneys. It is rapidly released by renal tubules after injury and increased in serum as well as urine soon after AKI. It is increased both in nephrotoxic and ischemic AKI (46).
Various studies have shown the diagnostic usefulness of NGAL as a marker of AKI, and it has been extensively studied in post-CABG AKI (47,48), but it can be used as a marker of AKI in patients with acute HF also.
Cystatin C
Cystatin C has been proposed as an ideal molecule to estimate GFR. In a prospective study, cystatin C and NGAL were measured in urine and serum of patients with AKI; the serum levels were not predictive of AKI within 6 h after surgery, but urinary levels were elevated, suggesting that urinary biomarkers may be superior to serum values in early detection of AKI (49).
Kidney injury molecule-1 (KIM-1)
KIM-1 is another marker, which increases in patients with ischemic and nephrotoxic AKI. Urinary KIM-1 is highly specific for ischemic AKI and not for CKD, prerenal AKI or contrast nephropathy (50,51).
IL-18 is a proinflammatory cytokine, which is detected in urine after ischemic proximal tubular injury. It shows good sensitivity and specificity for ischemic AKI (52).
Interleukin-18 (IL-18)
IL-18 is a proinflammatory cytokine, which is detected in urine after ischemic proximal tubular injury. It shows good sensitivity and specificity for ischemic AKI (52).
Despite good sensitivity and specificity of these markers, there are some limitations, like NGAL may be affected by preexisting renal diseases as well as infections. KIM-1 is specific for ischemic and nephrotoxic AKI and may not be useful for other causes of renal injury. IL-18 peaks at 4–6 h and more specific for ischemic injury and finally, cystatin C is not specific for ischemic AKI and increases in serum much later that other markers.
Another problem with these biomarkers is that these are not well-studied in patients with HF; most of data is with post-CABG AKI. These need validation in these patients before some recommendations can be made (7).
Another problem with these biomarkers is that these are not well-studied in patients with HF; most of data is with post-CABG AKI. These need validation in these patients before some recommendations can be made (7).
Bio-impedance Vector Analysis
Bio-impedance vector analysis gives better idea about hydration of patient with CRS and it can be used in combination with natriuretic peptide to guide the therapy in these patients.
Role of Imaging in Cardiorenal Syndrome
Imaging techniques have a major role in patients with CRS. These patients have high risk of deterioration in kidney functions if iodinated contrast media are used. So whenever possible, noninvasive techniques like stress echo or stress myocardial perfusion (SPECT, PET) should be used to diagnose ischemia along with cardiac enzymes (7).
Prevention of Cardiorenal Syndrome
The prevention of CRS is important because once CRS is set up, it is very difficult to interrupt, is not completely reversible always and is associated with serious adverse outcomes including need of hospitalization, dialysis and sometimes death (53). The pathophysiology of this disease is complex, so the preventive approaches should also be different in each syndrome.
Type I cardiorenal syndrome
The principal causes of type 1 CRS are ADHF and ACS leading to AKI. Of the patients who present with type 1 CRS, one-third are de novo cases, caused by pneumonia, hypertension, atrial fibrillation and acute ischemic events, etc. The remaining two-third of cases are patients with established HF, and CRS is precipitated by noncompliance with diet and medications of HF (54,55). Prevention can be achieved by proper use of angiotensin converting enzyme inhibitors (ACEI), angiotensin receptor blockers (ARB), beta-blockers, aldosterone receptor antagonists, adequate control of blood pressure, prevention of ACS via CAD risk modification and volume control by help of dietary restrictions and diuretics (7,53). A number of clinical trials have shown that HF can be prevented by patient’s education, weight monitoring and proper adherence to diet and medicines (56,57). A meta-analysis of 29 trials involving more than 5000 patients found that active intervention was associated with 26% less hospitalizations for HF as compared to controls (58). Once patient is admitted with HF then prompt treatment of underlying condition might prevent development of CRS type 1.
Chronic cardiorenal syndrome (Type 2)
Therapies to prevent type 2 CRS include proper use of ACEI/ARBs, aldosterone receptor antagonists, beta-blockers, vasodilators and cardiac resynchronization therapy (59,60). One of the most important preventive maneuvers is to control volume overload by fluid restriction, low salt diet and use of diuretics. Many studies have shown that the lowest doses of diuretics should be used to control symptoms and patients who require high doses of diuretics have the highest chances of developing CRS and have high mortality (61,62). In patients with low-output HF, anemia might cause decompensation and correction of anemia with erythropoietin has been shown to improve oxygen carrying capacity, left ventricular hypertrophy and ejection fraction in patients with CHF and CKD without survival benefits (63,64).
Lastly, use of nephrotoxic drugs like NSAIDs, aminoglycosides and contrast agents should be avoided in these patients (65).
Lastly, use of nephrotoxic drugs like NSAIDs, aminoglycosides and contrast agents should be avoided in these patients (65).
Acute renocardiac syndrome (Type 3)
Acute renocardiac syndrome is caused by AKI leading to acute cardiac dysfunction. It usually occurs after sudden volume overload or accelerated hypertension or hyperkalemia caused by AKI. It can be prevented by salt and fluid restriction and adequate use of renal replacement therapy including ultrafiltration whenever necessary (53). Sometimes AKI after contrast media and post cardiac surgery can also lead to type 3 CRS by causing AKI, which in turn would precipitate HF or arrhythmias. Adequate preventive strategies like hydration with saline or soda bicarbonate should be used before any contrast study, especially in patients with underlying CKD, elderly and other high-risk patients (66,67).
Chronic renocardiac syndrome (Type 4)
This is the most common type of CRS, as it is associated with CKD. The prevention of this syndrome lies in adequate control of diabetes, hypertension, etc., which cause CKD. It is seen in various studies that use of ACEI/ARB is beneficial in slowing the progression of diabetic nephropathy and proteinuric kidney diseases and slowing the progression of CKD (68). These agents can also reduce the incidence of cardiovascular disease in these patients. However, they are underused in CKD. Patients with CKD stage 5 on dialysis might develop recurrent ischemia and it has been seen that patients who have chronically high levels of cardiac biomarkers like troponins and NT pro-BNP have high chances of developing cardiac events, so these patients should be optimally managed with medications and revascularization (69,70). Fluctuation in volume status should be minimized, as this might lead to increased risk of cardiac systolic and diastolic dysfunction (71).
Type 5 cardiorenal syndrome
General approach includes adequate treatment of systemic condition causing cardiac and renal dysfunction, which improves function of both the organs (53).
Management of Cardiorenal Syndrome
Guidelines exist for management of HF and kidney disease separately; however, there are no guidelines to treat CRS. Recently ADQI group has reviewed the management based on available evidences (72).
Type 1 CRS
Initial management of patients with acute HF includes oxygen therapy to keep saturation above 90%, and noninvasive ventilation and morphine to relieve stress, anxiety and pain occasionally. Patients should be assessed clinically to see whether they have predominantly congestive symptoms or poor cardiac output or both (72). Treatment depends on underlying condition causing it, i.e., cardiac arrhythmias, myocardial infarction, hypertension, etc. In patients with ADHF, loop diuretic in higher doses are required mostly. Intravenous infusions are more effective than loading doses. Loop diuretics provide symptomatic relief, but overdiuresis and volume depletion can cause electrolyte imbalance like hypokalemia and reduce intravascular volume which lead to neurohormonal activation and further deterioration in kidney functions (73,74). So their doses should be adjusted accordingly.
Vasodilators like nitroglycerine and nesiritide are important agents to reduce congestion and preload (75). Nesiritide is a recombinant human B-type natriuretic peptide, which has vasodilator as well as mild diuretic property. In a small study, high-dose nesiritide was found to be useful in reducing pulmonary capillary wedge pressure (PCWP) and symptoms of HF in 57% of patients (76). However, in another study, regular and low doses of nesiritide (<0.03 to 0.015 μg/kg/min) were associated with worsening renal parameters in patients with ADHF. In a meta-analysis of five randomized trials, there was no difference in renal parameters when low-dose nesiritide was compared with standard treatment of diuretics and other vasodilators (77). Based on these data, nesiritide might be useful to improve symptoms in patients with HF, but worsening renal dysfunction is a concern and potential use of nesiritide is still under investigation (77,78).
Another class of drugs useful in ADHF is vasopressin receptor antagonist – vaptans. These agents improve hyponatremia by increasing free water excretion (72). Effect of tolvaptan – a V2 receptor antagonist – was studied in a prospective randomized trial (ACTIV) in 319 patients hospitalized with HF. Three doses of tolvaptan were used, i.e., 30, 60 and 90 mg/day and compared with placebo. It was seen that patients on tolvaptan 90 mg had significant reduction in weight, – 2.5 kg as compared to -0.6 kg within 24 h after randomization – but there was no difference in serum creatinine at discharge (79). In EVEREST trial, which was a larger study with >4000 patients, oral tolvaptan 30 mg/day was compared to placebo in patients with HF and serum creatinine >3.5 mg; results showed that there was a significant reduction in weight (-1.76 kg vs 0.97 kg) and improvement in dyspnea with tolvaptans. Serum sodium levels also increased significantly by 6 meq/L in tolvaptan group. However, there was no effect on mortality after a follow-up of 10 months (80).
Vasodilators like nitroglycerine and nesiritide are important agents to reduce congestion and preload (75). Nesiritide is a recombinant human B-type natriuretic peptide, which has vasodilator as well as mild diuretic property. In a small study, high-dose nesiritide was found to be useful in reducing pulmonary capillary wedge pressure (PCWP) and symptoms of HF in 57% of patients (76). However, in another study, regular and low doses of nesiritide (<0.03 to 0.015 μg/kg/min) were associated with worsening renal parameters in patients with ADHF. In a meta-analysis of five randomized trials, there was no difference in renal parameters when low-dose nesiritide was compared with standard treatment of diuretics and other vasodilators (77). Based on these data, nesiritide might be useful to improve symptoms in patients with HF, but worsening renal dysfunction is a concern and potential use of nesiritide is still under investigation (77,78).
Another class of drugs useful in ADHF is vasopressin receptor antagonist – vaptans. These agents improve hyponatremia by increasing free water excretion (72). Effect of tolvaptan – a V2 receptor antagonist – was studied in a prospective randomized trial (ACTIV) in 319 patients hospitalized with HF. Three doses of tolvaptan were used, i.e., 30, 60 and 90 mg/day and compared with placebo. It was seen that patients on tolvaptan 90 mg had significant reduction in weight, – 2.5 kg as compared to -0.6 kg within 24 h after randomization – but there was no difference in serum creatinine at discharge (79). In EVEREST trial, which was a larger study with >4000 patients, oral tolvaptan 30 mg/day was compared to placebo in patients with HF and serum creatinine >3.5 mg; results showed that there was a significant reduction in weight (-1.76 kg vs 0.97 kg) and improvement in dyspnea with tolvaptans. Serum sodium levels also increased significantly by 6 meq/L in tolvaptan group. However, there was no effect on mortality after a follow-up of 10 months (80).
Endothelin receptors blockers are not found to be useful in patients with HF and trials are ongoing for adenosine receptor blockers (81).
Patients who are resistant to diuretics, ultrafiltration might be required to reduce congestion. Ultrafiltration versus intravenous diuretics for the treatment of patients hospitalized for ADHF trial (UNLOAD) was a multicentric prospective randomized trial, which randomized 200 patients with ADHF and compared ultrafiltration with standard intravenous diuretic therapy (82). The primary outcomes were reduction in weight and dyspnea symptoms. After 90 days, the ultrafiltration group had less rehospitalization and greater net fluid loss (4.6 L as compared to 3.3 L with diuretics). There was no significant difference between serum creatinine and dyspnea score in two groups.
In patients with ACS and cardiogenic shock, inotropic agents are frequently required. Dopamine and dobutamine are usually used in these conditions. Levosimendan belongs to a new class of inotropic drugs called calcium sensitizers. A randomized trial showed moderate to marked improvement in patients treated with levosimendan (83). Sometimes systemic vasoconstrictors like norepinephrine are needed to increase blood pressure. Intra-aortic balloon pump is required sometimes to augment cardiac output. Left ventricular assist device may be used in certain patients as a bridge to cardiac transplantation (84).
In patients with ACS and cardiogenic shock, inotropic agents are frequently required. Dopamine and dobutamine are usually used in these conditions. Levosimendan belongs to a new class of inotropic drugs called calcium sensitizers. A randomized trial showed moderate to marked improvement in patients treated with levosimendan (83). Sometimes systemic vasoconstrictors like norepinephrine are needed to increase blood pressure. Intra-aortic balloon pump is required sometimes to augment cardiac output. Left ventricular assist device may be used in certain patients as a bridge to cardiac transplantation (84).
Type 2 CRS
Therapeutic approach to patients with CHF includes treatment of underlying disease, regular medications and adherence to diet and exercise (72).
Pharmacological therapy includes use of ACEI/ARBs and beta-blockers and aldosterone receptor antagonists. These agents significantly reduce morbidity and mortality (85–88). Caution is required when using combination of ACEI/ARB and aldosterone receptor antagonist, as it may cause hyperkalemia. So a dietary advice should always be given along with monitoring of serum potassium and renal function in these patients. The combination of ACEI and ARB has shown to improve outcomes (89) but ONTARGET trial did not show any additional benefit of combining ARBs with ACEI and had higher chances of hyperkalemia (90). Similarly, a combination of all four neuroendocrine blockers (ACEI, ARB, beta-blockers and aldosterone antagonists) is not recommended. Digoxin and diuretics provide symptomatic relief, but they have no survival benefit (91).
Pharmacological therapy includes use of ACEI/ARBs and beta-blockers and aldosterone receptor antagonists. These agents significantly reduce morbidity and mortality (85–88). Caution is required when using combination of ACEI/ARB and aldosterone receptor antagonist, as it may cause hyperkalemia. So a dietary advice should always be given along with monitoring of serum potassium and renal function in these patients. The combination of ACEI and ARB has shown to improve outcomes (89) but ONTARGET trial did not show any additional benefit of combining ARBs with ACEI and had higher chances of hyperkalemia (90). Similarly, a combination of all four neuroendocrine blockers (ACEI, ARB, beta-blockers and aldosterone antagonists) is not recommended. Digoxin and diuretics provide symptomatic relief, but they have no survival benefit (91).
Cardiac resynchronization therapy is nowadays recommended to symptomatic patients with NYHA class III and IV HF, poor left ventricular ejection fraction (LVEF) and QRS prolongation (92,93). Implantable defibrillators are useful in survivor of cardiac arrest, patients with recurrent ventricular arrhythmias and also in patients with HF with poor LVEF. In selected patients with no response to these therapies, mechanical assist devices and/or cardiac transplantation may be useful (94).
In patients with right sided HF, the treatment depends on whether it is underfilled or overfilled. Treatment should be directed toward underlying causes of right sided failure.
Patients having concomitant CKD require loop diuretics as thiazides are less effective in these patients. Sometimes a combination of these two agents is required, but it can cause severe electrolyte disturbances like hypokalemia and hyponatremia due to sequential action of these agents. Diuretic infusion is more effective than bolus injections. In patients refractory to these agents, renal replacement therapy may be required. Use of ACEI/ARB can sometimes cause hyperkalemia and renal function deterioration in these patients, so a careful monitoring is required.
Anemia is frequently present in these patients and its correction may improve symptoms without improving survival. Nephrotoxic drugs like NSAIDs and aminoglycosides should be avoided in these patients. The doses of many renally excreted drugs, for example, digoxin and allopurinol, should be reduced accordingly in these patients.
Patients having concomitant CKD require loop diuretics as thiazides are less effective in these patients. Sometimes a combination of these two agents is required, but it can cause severe electrolyte disturbances like hypokalemia and hyponatremia due to sequential action of these agents. Diuretic infusion is more effective than bolus injections. In patients refractory to these agents, renal replacement therapy may be required. Use of ACEI/ARB can sometimes cause hyperkalemia and renal function deterioration in these patients, so a careful monitoring is required.
Anemia is frequently present in these patients and its correction may improve symptoms without improving survival. Nephrotoxic drugs like NSAIDs and aminoglycosides should be avoided in these patients. The doses of many renally excreted drugs, for example, digoxin and allopurinol, should be reduced accordingly in these patients.
Chronic renocardiac syndrome (Type 4)
CKD often leads to multiple cardiac problems like chronic volume overload which can lead to HF and accelerated hypertension. So dietary restriction of fluid and salt is required in these patients. Adequate control of blood pressure is another important aspect. Correction of anemia is associated with improvement in symptoms as well as reduction in LVH in some studies without survival benefit. Despite benefit, use of ARB/ACEI and beta-blockers is less in patients with CKD; these agents should be used whenever tolerated (95). Loop diuretics are often necessary.
Conclusions
CRS is a complex disorder involving both heart and kidneys. The classification of this syndrome in various subgroups would help in better identification and management of problem. The CRS type 1 is most well-known type of cardiorenal disorder in clinical practice; however, the epidemiology of other types of CRSs is not so well defined. There is important role of neuroendocrine system in pathophysiology of this syndrome and similarly agents which block these responses are found to be useful in these syndromes. There is an important role of diet and salt restriction in addition to drugs in management. Novel biomarkers, which have been used to diagnose AKI and HF may be useful in early diagnosis of this syndrome, which might help to prevent the progression of complication.
References
References
- Cardiovascular Disease. http://www.americanheart.org/ [Accessed on September, 2008].
- Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, Van Lente F, Levey AS. Prevalence of chronic kidney disease in the United States. J Am Med Assoc. 2007; 298(17):2038–47.
- Foley RN, Murray AM, Li S, Herzog CA, McBean AM, Eggers PW, Collins AJ. Chronic kidney disease and the risk for cardiovascular disease, renal replacement, and death in the United States medicare population, 1998 to 1999. J Am Soc Nephrol. 2005; 16(2):489–95.
- Logar CM, Herzog, Beddhu S. Diagnosis and therapy of coronary artery disease in renal failure, end-stage renal disease, and renal transplant populations. Am J Med Sci. 2003; 325(4):214–27.
- Logeart D, Tabe JY, Hittinger L, Thabut G, Jourdain P, Maison P, Tartiere JM, Solal AC. Transient worsening of renal function during hospitalization for acute heart failure alters outcome. Int J Cardiol. 2008; 127(2):228–32.
- Ronco C, Haapio M, House AA, Anavekar N, Bellomo R. Cardiorenal syndrome. J Am Coll Cardiol. 2008; 52:1527–39.
- Ronco C, McCullough P, Anker SD, Anand I, Aspromonte N, Bagshaw SM, Bellomo R, Berl T, Bobek I, Cruz DN, Daliento L, Davenport A, Haapio M, Hillege H, House AA, Katz N, Maisel A, Mankad S, Zanco P, Mebazaa A, Palazzuoli A, Ronco F, Shaw A, Sheinfeld G, Soni S, Vescovo G, Zamperetti N, Ponikowski P; Acute Dialysis Quality Initiative (ADQI) consensus group. Cardio-renal syndromes: report from the consensus conference of the acute dialysis quality initiative. Eur Heart J. 2010; 31(6):703–11.
- House AA, Anand I, Bellomo R. Definition and classification of cardio-renal syndromes: workgroup statements from the 7th ADQI Consensus Conference. Nephrol Dial Transplant. 2010; 25:1416–20.
- Cruz1 DN, Bagshaw SM. Heart–kidney interaction: epidemiology of cardiorenal syndrome. Int J Nephrol. 2011; 351291:11.
- Forman DE, Butler J, Wang Y, Abraham WT, O’Connor CM, Gottlieb SS, Loh E, Massie BM, Rich MW, Stevenson LW, Young JB, Krumholz HM. Incidence, predictors at admission, and impact of worsening renal function among patients hospitalized with heart failure. J Am Coll Cardiol 2004; 43:61–7.
- Gottlieb SS, Abraham W, Butler J, Forman DE, Loh E, Massie BM, O’connor CM, Rich MW, Stevenson LW, Young J, Krumholz HM. The prognostic importance of different definitions of worsening renal function in congestive heart failure. J Cardiac Failure. 2002; 8(3):136–41.
- Newsome BB, Warnock DG, McClellan WM, Herzog CA, Kiefe CI, Eggers PW, Allison JJ. “Long-term risk of mortality and end-stage renal disease among the elderly after small increases in serum creatinine level during hospitalization for acute myocardial infarction. Arch Intern Med. 2008; 168(6):609–16.
- Parikh CR, Coca SG, Wang Y, Masoudi FA, Krumholz HM. Long-term prognosis of acute kidney injury after acute myocardial infarction. Arch Intern Med. 2008; 168(9):987–95.
- Cowie MR, Komajda M, Murray-Thomas T, Underwood J, Ticho B. Prevalence and impact of worsening renal function in patients hospitalized with decompensated heart failure: results of the prospective outcomes study in heart failure (POSH). Eur Heart J. 2006; 27(10):1216–22.
- Khan NA, Ma I, Thompson CR, Humphries K, Salem DN, Sarnak MJ, Levin A. Kidney function and mortality among patients with left ventricular systolic dysfunction. J Am Soc Nephrol. 2006; 17(1):244–53.
- Ronco C, Levin A, Wanock DG, Mehta R, Kellum JA, Shah S, Molitoris BA. Improving outcomes of acute kidney injury (AKI): report on an initiative. Int J Artif Organs. 2007; 30:373–6.
- Bagshaw SM, Cruz DN, Aspromonte N, Acute Dialysis Quality Initiative (ADQI) Consensus Group. Epidemiology of cardio-renal syndromes: workgroup statements from the 7th ADQI Consensus Conference. Nephrol Dial Transplant. 2010; 25:1406–16.
- Adams KF, Jr, Fonarow GC, Emerman CL, LeJemtel TH, Costanzo MR, Abraham WT, Berkowitz RL, Galvao M, Horton DP; ADHERE Scientific Advisory Committee and Investigators. Characteristics and outcomes of patients hospitalised for heart failure in the United States: rationale, design and preliminary observations from the first 100,000 cases in the Acute Decompensated Heart Failure National Registry (ADHERE). Am Heart J. 2005; 149: 209–16.
- Heywood JT, Fonarow GC, Costanzo MR, Mathur VS, Wigneswaran JR, Wynne J. High prevalence of renal dysfunction and its impact on outcome in 118,465 patients hospitalized with acute decompensated heart failure: a report from the ADHERE Database. J Cardiac Failure. 2007; 13(6):422–30.
- Elsayed EF, Tighiouart H, Griffith J, Kurth T, Levey AS, Salem DN, Sarnak MJ, Weiner DE. Cardiovascular disease and subsequent kidney disease. Arch Intern Med. 2007; 167(11):1130–6.
- Ahmed A, Rich MW, Sanders PW, Perry GJ, Bakris GL, Zile MR, Love TE, Aban IB, Shlipak MG. Chronic kidney disease associated mortality in diastolic versus systolic heart failure: a propensity matched study. Am J Cardiol. 2007; 99(3):393–8.
- Campbell RC, Sui X, Filippatos G, Love TE, Sanders PW, Ahmed A. Association of chronic kidney disease with outcomes in chronic heart failure: a propensity-matched study. Nephrol Dialysis Transplant. 2009; 24(1):186–93.
- Elsayed EF, Tighiouart H, Griffith J, Kurth T, Levey AS, Salem DN, Sarnak MJ, Weiner DE. Cardiovascular disease and subsequent kidney disease. Arch Intern Med. 2007; 167:1130–6.
- Dimopoulos K, Diller G. Prevalence, predictors and prognostic value of renal dysfunction in adults with congenital heart disease. Circulation. 2008; 117:2320–8.
- Santos MP, Vilacosta I. Cardiorenal syndrome: an unsolved clinical problem. Int J Nephrol. 2011; 913029:6.
- Bock JS, Gottlieb SS. Cardiorenal syndrome: new perspectives. Circulation. 2010; 121(23):2592–600.
- Chabrashvili T, Kitiyakara C, Blau J, Karber A, Aslam S, Welch WJ, Wilcox CS. Effects of ANG II type 1 and 2 receptors on oxidative stress, renal NADPH oxidase, and SOD expression. Am J Physiol Regul Integr Comp Physiol. 2003; 285(1):R117–24.
- Nohria A, Hasselblad V, Stebbins A, Pauly DF, Fonarow GC, Shah M, Yancy CW, Califf RM, Stevenson LW, Hill JA. Cardiorenal interactions. Insights from the ESCAPE trial. J Am Coll Cardiol. 2008; 51(13):1268–74.
- Mullen W, Abrahams Z, Francis GS, Sokos G, Taylor DO, Starling RC, Young JB, Tang WH. Importance of venous congestion for worsening of renal function in advanced decompensated heart failure. J Am Coll Cardiol. 2009; 53(7):589–96.
- Damman K, Navis G, Smilde TD, Voors AA, van der Bij W, van Veldhuisen DJ, Hillege HL. Decreased cardiac output, venous congestion and the association with renal impairment in patients with cardiac dysfunction. Eur J Heart Failure. 2007; 9(9):872–8.
- McCullough PA, Wolyn R, Rocher LL, Levin RN, O’Neill WW. Acute renal failure after coronary intervention: incidence, risk factors, and relationship to mortality. Am J Med. 1997; 103:368–75.
- Rihal CS, Textor SC, Grill DE. Incidence and prognostic importance of acute renal failure after percutaneous coronary intervention. Circulation. 2002; 105:2259–64.
- Herzog CA. Dismal long-term survival of dialysis patients after acute myocardial infarction: can we alter the outcome? Nephrol Dial Transplant. 2002; 17:7–10.
- McCullough PA, Li S. Chronic kidney disease, prevalence of premature cardiovascular disease, and relationship to short-term mortality. Am Heart J. 2008; 156:277–83.
- Yerkey MW, Kernis SJ. Renal dysfunction and acceleration of coronary disease. Heart. 2004; 90:961–66.
- Bagshaw SM, Lapinsky S, Dial S, Arabi Y, Dodek P, Wood G, Ellis P, Guzman J, Marshall J, Parrillo JE, Skrobik Y, Kumar A; Cooperative Antimicrobial Therapy of Septic Shock (CATSS) Database Research Group. Acute kidney injury in septic shock: clinical outcomes and impact of duration of hypotension prior to initiation of antimicrobial therapy. Intensive Care Med. 2009; 35:871–81.
- Oppert M, Engel C, Brunkhorst FM, Bogatsch H, Reinhart K, Frei U, Eckardt K-U, Loeffler M, John S, for the German Competence Network Sepsis (Sepnet). Acute renal failure in patients with severe sepsis and septic shock a significant independent risk factor for mortality: results from the German Prevalence Study. Nephrol Dial Transplant. 2008; 23:904–9.
- Bagshaw SM, Uchino S, Bellomo R, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Macedo E, Gibney N, Tolwani A, Oudemans-Straaten HM, Ronco C, Kellum JA. Septic acute kidney injury in critically ill patients: clinical characteristics and outcomes. Clin J Am Soc Nephrol. 2007; 2:431–9.
- Neveu H, Kleinknecht D, Brivet F, Loirat P, Landais P. Prognostic factors in acute renal failure due to sepsis. Results of a prospective multicentre study. The French Study Group on Acute Renal Failure. 1996; 11:293–9.
- Metha NJ, Khan IA, Gupta V. Cardiac troponin predicts myocardial dysfunction and adverse outcome in septic shock. Int J Cardiol. 2004;95: 13–7.
- Ammann P, Maggiorinin M, Bertel O. Troponin as a risk factor for mortality in critically ill patients without acute coronary syndromes. J Am Coll Cardiol. 2003; 41:2004–9.
- Meyer B, Huelsmann M, Wexberg P, Delle Karth G, Berger R, Moertl D, Szekeres T, Pacher R, Heinz G. N-terminal pro-B-type natriuretic peptide is an independent predictor of outcome in an unselected cohort of critically ill patients. Crit Care Med. 2007; 35:2268–73.
- Morrow DA, de Lemos JA, Blazing MA, Sabatine MS, Murphy SA, Jarolim P, White HD, Fox KA, Califf RM, Braunwald E. Prognostic value of serial B-type natriuretic peptide testing during follow-up of patients with unstable coronary artery disease. J Am Med Assoc. 2005; 294:2866–71.
- Carr SJ, Bavanandan S, Fentum B, Ng L. Prognostic potential of brain natriuretic peptide (BNP) in predialysis chronic kidney disease patients. Clin Sci (Lond). 2005; 109:75–82.
- Austin WJ, Bhalla V, Hernandez-Arce I, Isakson SR, Beede J, Clopton P, Maisel AS, Fitzgerald RL. Correlation and prognostic utility of B-type natriuretic peptide and its amino-terminal fragment in patients with chronic kidney disease. Am J Clin Pathol. 2006; 126:506–12.
- Xu S, Venge P. Lipocalins as biochemical markers of disease. Biochim Biophys Acta. 2000; 1482:298–307.
- Mishra J, Mori K, Ma Q, Kelly C, Barasch J, Devarajan P. Neutrophil gelatinase-associated lipocalin: a novel early urinary biomarker for cisplatin nephrotoxicity. Am J Nephrol. 2004; 24:307–15.
- Mori K, Nakao K. Neutrophil gelatinase-associated lipocalin as the real-time indicator of active kidney damage. Kidney Int. 2007; 71:967–70.
- Herget-Rosenthal S, Marggraf G, Husing J, Goring F, Pietruck F, Janssen O, Philipp T, Kribben A. Early detection of acute renal failure by serum cystatin C. Kidney Int. 2004; 66:1115–22.
- Han WK, Bailly V, Abichandani R, Thadhani R, Bonventre JV. Kidney injury molecule-1 (KIM-1): a novel biomarker for human renal proximal tubule injury. Kidney Int. 2002; 62:237–44.
- Ichimura T, Hung CC, Yang SA, Stevens JL, Bonventre JV. Kidney injury molecule-1: a tissue and urinary biomarker for nephrotoxicant-induced renal injury. Am J Physiol Renal Physiol. 2004; 286:F552–63.
- Parikh CR, Jani A, Melnikov VY, Faubel S, Edelstein CL. Urinary interleukin-18 is a marker of human acute tubular necrosis. Am J Kidney Dis. 2004; 43:405–14.
- McCullough PA, Haapio M, Mankad S, Zamperetti N, Massie B, Bellomo R, Berl T, Anker SD, Anand I, Aspromonte N, Bagshaw SM, Bobek I, Cruz DN, Daliento L, Davenport A, Hillege H, House AA, Katz N, Maisel A, Mebazaa A, Palazzuoli A, Ponikowski P, Ronco F, Shaw A, Sheinfeld G, Soni S, Vescovo G, Zanco P, Ronco C, Berl T; Acute Dialysis Quality Initiative (ADQI) Consensus Group. Prevention of cardio-renal syndromes: workgroup statements from the 7th ADQI Consensus Conference. Nephrol Dial Transplant. 2010; 25:1777–84.
- Fonarow GC, Abraham WT, Albert NM, Stough WG, Gheorghiade M, Greenberg BH, O’Connor CM, Pieper K, Sun JL, Yancy CW, Young JB; OPTIMIZE-HF Investigators and Hospitals. Factors identified as precipitating hospital admissions for heart failure and clinical outcomes: findings from OPTIMIZE-HF. Arch Intern Med. 2008; 168:847–54.
- Ghali JK, Kadakia S, Cooper R, Ferlinz J. Precipitating factors leading to decompensation of heart failure traits among urban blacks. Arch Intern Med. 1988; 148: 2013–6.
- López Cabezas C, Falces Salvador C, Cubí Quadrada D, Arnau Bartés A, Ylla Boré M, Muro Perea N, Muro Perea N, Homs Peipoch E. Randomized clinical trial of a postdischarge pharmaceutical care program vs regular follow-up in patients with heart failure. Farm Hosp. 2006; 30:328–42.
- Murray MD, Young J, Hoke S, Tu W, Weiner M, Morrow D, Stroupe KT, Wu J, Clark D, Smith F, Gradus-Pizlo I, Weinberger M, Brater DC. Pharmacist intervention to improve medication adherence in heart failure: a randomized trial. Ann Intern Med. 2007; 146:714–25.
- McAlister FA, Stewart S, Ferrua S, McMurray JJ. Multidisciplinary strategies for the management of heart failure patients at high risk for admission: a systematic review of randomized trials. J Am Coll Cardiol. 2004; 44:810–9.
- Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG, Jessup M, Konstam MA, Mancini DM, Michl K, Oates JA, Rahko PS, Silver MA, Stevenson LW, Yancy CW; American College of Cardiology Foundation; American Heart Association. ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure): developed in collaboration with the American College of Chest Physicians and the International Society for Heart and Lung Transplantation: endorsed by the Heart Rhythm Society. J Am Coll Cardiol. 2005; 46:e1–82.
- Boerrigter G, Costello-Boerrigter LC, Abraham WT, St. John Sutton MG, Heublein D, Kruger KM, Hill MR, McCullough PA, Burnett JC. Cardiac resynchronization therapy with biventricular pacing improves renal function in heart failure patients with reduced glomerular filtration rate. Circulation. 2007;116: II-405.
- Hasselblad V, Gattis Stough W, Shah MR, Lokhnygina Y, O’Connor CM, Califf RM, Adams KF, Jr. Relation between dose of loop diuretics and outcomes in a heart failure population: results of the ESCAPE trial. Eur J Heart Fail. 2007; 9:1064–9.
- Ahmed A, Husain A, Love TE, Gambassi G, Dell’Italia LJ, Francis GS, Gheorghiade M, Allman RM, Meleth S, Bourge RC. Heart failure, chronic diuretic use, and increase in mortality and hospitalization: an observational study using propensity score methods. Eur Heart J. 2006; 27:1431–9.
- McCullough PA, Lepor NE. The deadly triangle of anemia, renal insufficiency, and cardiovascular disease: implications for prognosis and treatment. Rev Cardiovasc Med. 2005; 6:1–10.
- Jones M, Schenkel B, Just J. Epoetin alfa’s effect on left ventricular hypertrophy and subsequent mortality. Int J Cardiol. 2005; 100:253–65.
- Mukherjee D. Nonsteroidal anti-inflammatory drugs and the heart: what is the danger? Congest Heart Fail. 2008; 14:75–82.
- Marenzi G, Bartorelli AL. Recent advances in the prevention of radiocontrast-induced nephropathy. Curr Opin Crit Care. 2004; 10:505–9.
- Schetz M, Bove T, Morelli A, Mankad S, Ronco C, Kellum JA. Prevention of cardiac surgery-associated acute kidney injury. Int J Artif Organs. 2008; 31:179–89.
- de Zeeuw D, Remuzzi G, Parving HH, Keane WF, Zhang Z, Shahinfar S, Snapinn S, Cooper ME, Mitch WE, Brenner BM. Albuminuria, a therapeutic target for cardiovascular protection in Type 2 diabetic patients with nephropathy. Circulation. 2004; 110:921–7.
- deFilippi CR, Thorn EM, Aggarwal M, Joy A, Christenson RH, Duh SH, Jeudy J, Beache G. Frequency and cause of cardiac troponin T elevation in chronic hemodialysis patients from study of cardiovascular magnetic resonance. Am J Cardiol. 2007; 100:885–9.
- McCullough PA. Evaluation and treatment of coronary artery disease in patients with end-stage renal disease. Kidney Int Suppl. 2005; 95:51–s58.
- Dumler F, McCullough PA. Optimal dialysis for the end-stage renal disease patient with cardiovascular disease. Adv Chronic Kidney Dis. 2004; 11:261–73.
- Davenport A, Anker SD, Mebazaa A, et al. ADQI 7: the clinical management of the cardio-renal syndromes: work group statements from the 7th ADQI consensus conference. Nephrol Dial Transplant. 2010; 25:2077–89.
- Wang DJ, Gottlieb SS. Diuretics: still the mainstay of treatment. Crit Care Med. 2008; 36:S89–94.
- Milo-Cotter O, Sasimangalam AN, Arumugham PS, Kaluski E , Weatherley B, Cotter G. Diuretics: a panacea for acute heart failure? Different formulations, doses, and combinations. Heart Fail Monit. 2008; 6:9–19.
- Hollenberg SM. Vasodilators in acute heart failure. Heart Fail Rev. 2007; 12:143–7.
- Colucci WS, Elkayam U, Horton DP, Abraham WT, Bourge RC, Johnson AD, Wagoner LE, Givertz MM, Liang CS, Neibaur M, Haught WH, LeJemtel TH. Intravenous nesiritide, a natriuretic peptide, in the treatment of decompensated congestive heart failure. Nesiritide Study Group. N Engl J Med. 2000; 343:246–53.
- Sackner-Bernstein JD, Skopicki HA, Aaronson KD. Risk of worsening renal function with nesiritide in patients with acutely decompensated heart failure. Circulation. 2005; 111:1487–91.
- Owan TE, Chen HH, Frantz RP, Karon BL, Miller WL, Rodeheffer RJ, Hodge DO, Burnett JC, Jr, Redfield MM. The effects of nesiritide on renal function and diuretic responsiveness in acutely decompensated heart failure patients with renal dysfunction. J Card Fail. 2008; 14:267–75.
- Gheorghiade M, Gattis WA, O’Connor CM, Adams KF, Jr, Elkayam U, Barbagelata A, Ghali JK, Benza RL, McGrew FA, Klapholz M, Ouyang J, Orlandi C, Acute and Chronic Therapeutic Impact of a Vasopressin Antagonist in Congestive Heart Failure (ACTIV in CHF) Investigators: effects of tolvaptan, a vasopressin antagonist, in patients hospitalized with worsening heart failure. A randomized controlled trial. JAMA. 2004; 291:1963–71.
- Konstam MA, Gheorghiade M, Burnett JC, Jr, Grinfeld L, Maggioni AP, Swedberg K, Udelson JE, Zannad F, Cook T, Ouyang J, Zimmer C, Orlandi C. Efficacy of Vasopressin Antagonism in Heart Failure Outcome Study with Tolvaptan (EVEREST) Investigators: effects of oral tolvaptan in patients hospitalized for worsening heart failure. The EVEREST Outcome Trial. JAMA. 2007; 297:1319–31.
- Givertz MM, Massie BM, Fields TK, Pearson LL, Dittrich HC; CKI-201 and CKI-202 Investigators. The effects of KW-3902, an adenosine A1-receptor antagonist, on diuresis and renal function in patients with acute decompensated heart failure and renal impairment or diuretic resistance. J Am Coll Cardiol. 2007; 50:1551–660.
- Costanzo MR, Guglin ME, Saltzberg MT, Jessup ML, Bart BA, Teerlink JR, Jaski BE, Fang JC, Feller ED, Haas GJ, Anderson AS, Schollmeyer MP, Sobotka PA for the UNLOAD Trial Investigators. Ultrafiltration versus intravenous diuretics for patients hospitalized for acute decompensated heart failure. J Am Coll Cardiol. 2007; 49:675–83.
- Yilmaz MB, Yalta K, Yontar C, Karadas F, Erdem A, Turgut OO, Yilmaz A, Tandogan I. Levosimendan improves renal function in patients with acute decompensated heart failure: comparison with dobutamine. Cardiovasc Drugs Ther. 2007; 21:431–5.
- Arora RR, Shah AG. Enhanced external counterpulsation: a new modality in the treatment of angina and heart failure. J Cardiovasc Pharmacol Ther. 2006; 11:271–3.
- The SOLVD Investigators. Effect of enalapril on survival in patients with reduced left ventricular ejection fraction and congestive heart failure. N Engl J Med. 1991; 325:293–302.
- McAlister FA, Stewart S, Fettua S, McMurray JJ. Multidisciplinary strategies for the management of heart failure patients at high risk for admission: a systematic review of randomised trials. J Am Coll Cardiol. 2004; 44:810–9.
- Bangalore S, Messerli FH, Kostis JB, Pepine CJ. Cardiovascular protection using beta-blockers: a critical review of the evidence. J Am Coll Cardiol. 2007; 50:563–72.
- Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A, Palensky J, Wittes J. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomised Aldactone Evaluation Study Investigators. N Engl J Med. 1999; 341:709–17.
- Lakhdar R, Al-Mallah MH, Lanfear DE. Safety and tolerability of angiotensin-converting enzyme inhibitor versus the combination of angiotensin-converting enzyme inhibitor and angiotensin receptor blocker in patients with left ventricular dysfunction: a systematic review and meta-analysis of randomized controlled trials. J Card Fail. 2008; 14:181–8.
- Cowan BR, Young AA, Anderson C, Doughty RN, Rungroj K, Eva L, Thomas MH, Chris RM, John SE, Roland SE, Koon T, Angela WK, Stephen WG, Cheuk-Man Y, Salim Y, Garry JL, ONTARGET Investigators. Left ventricular mass and volume with telmisartan, ramipril, combination in patients with previous atherosclerotic events or with diabetes mellitus (from the Ongoing Telmisartan Alone and in combination with Ramipril Global Endpoint Trial (ONTARGET). Am J Cardiol. 2009; 104:1484–9.
- The Digitalis Investigation Group. The effect of digoxoin on mortality and morbidity in patients with heart failure. N Engl J Med. 1997; 336:525–33.
- Vardas PE, Auricchio A, Blanc JJ, Daubert JC, Drexler H, Ector H, Gasparini M, Linde C, Morgado FB, Oto A, Sutton R, Trusz-Gluza M, European Society of Cardiology, European Heart Rhythm Association. Guidelines for cardiac pacing and cardiac resynchronization therapy: the task force for cardiac pacing and cardiac resynchronization therapy of the European Society of Cardiology. Developed in collaboration with the European Heart Rhythm Association. Eur Heart J. 2007; 28:2256–95.
- Barnett D, Phillips S, Longson C. Cardiac resynchronisation therapy for the treatment of heart failure: NICE technology appraisal guidance. Heart. 2007; 93:1134–5.
- European Society of Cardiology, Heart Failure Association of the ESC (HFA), European Society of Intensive Care Medicine (ESICM), et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008. Eur J Heart Fail 2008; 10:933–89.
- Gowdak LH, Arantes RL, de Paula FJ, Krieger EM, De Lima JJ. Underuse of American College of Cardiology/American Heart Association Guidelines in hemodialysis patients. Ren Fail. 2007; 29:559–65.
- Why Publish with JCPC?
- Instructions to the Authors
- Submit Manuscript
- Advertise with Us
- Journal Scientific Committee
- Editorial Policy
Print: ISSN: 2250-3528


