The Journal of Clinical and Preventive Cardiology has moved to a new website. You are currently visiting the old
website of the journal. To access the latest content, please visit www.jcpconline.org.
Case Vignettes
Cardiac Evaluation Leading to Diagnosis of Non-cardiac Illnesses
Volume 2, Jul 2013
Divya Malhotra, FACC, FASE, Madhu Mary, MD, Ravi R Kasliwal, MD, DM, Gurgaon, Haryana, India
J Clin Prev Cardiol. 2013;2(3):168-9
A proper and successful clinical examination requires close attention to be paid to all clinical details, irrespective of one’s specialty or the patient’s presenting symptoms. Often, subtle clues can be picked during clinical evaluation that prove vital in reaching correct diagnoses, which would not have been even thought of based on the clinical presentation. We hereby describe two such cases in which cardiac evaluation led to the diagnosis of underlying non-cardiac pathologies.
Case 1
A 27-year-old gentleman came to the clinic with complaints of left sided chest pain and a sensation of heaviness on and off starting the night before. The pain had no relation to exertion. He denied any history of shortness of breath but reported that he used to go to the gym regularly and did moderate work out.
He was seen at a local hospital the night before and had a negative cardiac troponin test.
The patient came the next morning for a stress echocardiography (echo) to our clinic. A baseline echo was first obtained but it was limited by a very poor acoustic window. Both the apical and parasternal images were very difficult to obtain. Hence, the echo images were obtained from the subcostal view, which confirmed normal orientation of the cardiac chambers in the left chest cavity. The poor echo images was rather surprising as the patient was not obese, only smoked occasionally and was not known to have chronic obstructive pulmonary disease. He had mild chest heaviness even while standing on the treadmill and this increased when he started walking on it. Consequently, orgthe exercise was stopped prematurely after 5 minutes. There were no significant ECG changes at peak exercise and the echo images obtained from the subcostal view were also normal.
In view of the poor acoustic window in a normally built patient and without any reasonable explanation, a diagnosis of pneumothorax was suspected as air is bad conductor of ultrasound waves. Chest X-ray was obtained which revealed a linear shadow in the left lower hemithorax with paucity of bronchovascular markings (Figure 1, marked with arrow), consistent with pneumothorax.
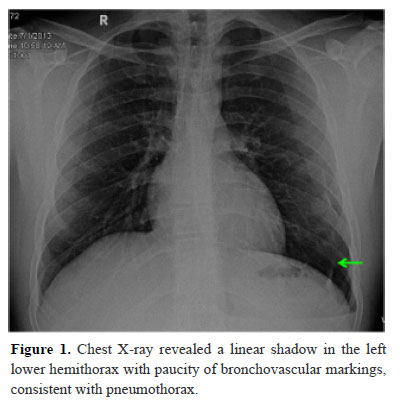
In view of the poor acoustic window in a normally built patient and without any reasonable explanation, a diagnosis of pneumothorax was suspected as air is bad conductor of ultrasound waves. Chest X-ray was obtained which revealed a linear shadow in the left lower hemithorax with paucity of bronchovascular markings (Figure 1, marked with arrow), consistent with pneumothorax.
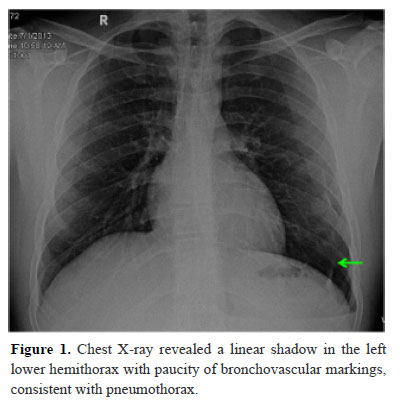
This case reemphasizes the importance of seeing a patient in totality. If the echo images cannot be obtained optimally in a patient with chest pain, in absence of obstructive airway disease or obesity and with normal orientation of cardiac chambers, then a diagnosis of pneumthorax should be considered.
Case 2
A 55-year-old lady with recently diagnosed hypertension came to the clinic for an ECG. She reported that for the last two days she was having a headache and feeling of nausea and vomiting. She was seen by her family physician who prescribed her an antiemetic for nausea. The nausea was better, but headache persisted and she had now developed epigastric discomfort also for which an ECG was sought.
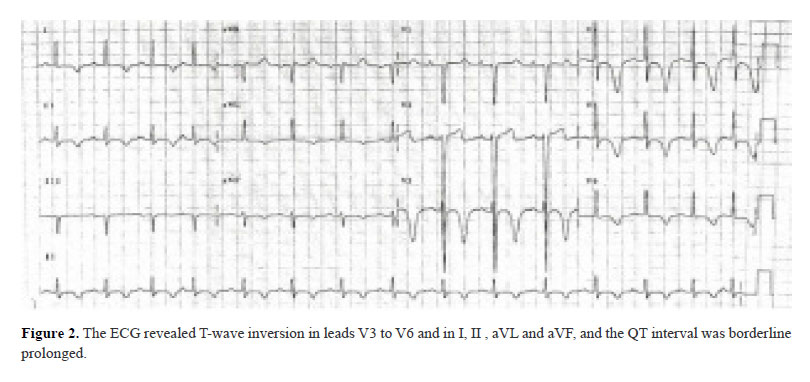
The ECG revealed T-wave inversion in leads V3 to V6 and in I, II , aVL and aVF, and the QT interval was borderline prolonged (Figure 2). In comparison to her previous ECG the above changes were new. On interviewing the patient it was discovered that the headache was severe. On physical examination neck stiffness was present. In view of the clinical findings and ECG changes, the diagnosis of subarachnoid hemorrhage (SAH) was suspected. The patient was urgently sent for a computed tomographic scan of the head which revealed a subarachnoid bleed.
- Why Publish with JCPC?
- Instructions to the Authors
- Submit Manuscript
- Advertise with Us
- Journal Scientific Committee
- Editorial Policy
Print: ISSN: 2250-3528


